Press around the “male fertility crisis” — also dubbed “spermageddon” — has drawn attention to the global decline in sperm counts. Some researchers predict catastrophic outcomes if nothing changes. However, the recent findings are not without debate among the experts in male fertility. Naturally, this can cause confusion among the general public. Should you be worried about the male fertility crisis? And what could be the cause?
While there is more research yet to be done, we’ll summarize what the existing studies show, evaluate their conclusions, and offer insights into some of the reasons behind the decline in male fertility.
Fertility is decreasing globally
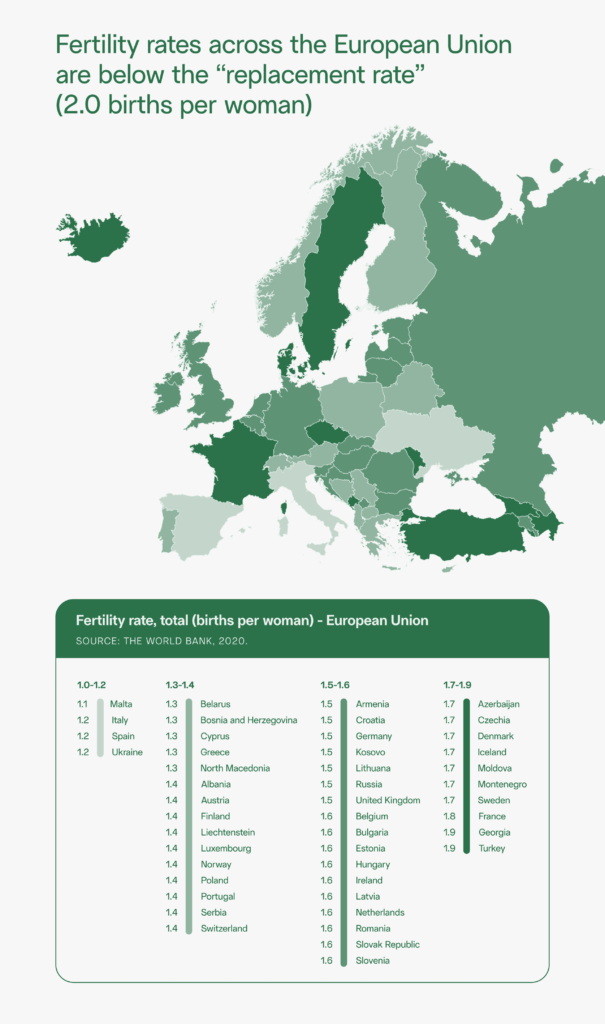
A population’s “fertility” is measured by the number of children born per adult woman. According to the US Population Reference Bureau’s 2021 Data Sheet, fertility is down worldwide, regardless of a country’s economic status.
In 2019, fertility rates reached an all-time low of 1.7 children per woman (or 55.8 children per 1,000 women). Provisional data suggests that — likely due to the COVID-19 pandemic — US birth rates declined by a further 4% in 2020.
However, as mentioned, this isn’t just an American problem. Fertility rates in the United Kingdom have been declining for over a decade, currently hovering at around 1.6 children per woman. Not a single country in the European Union has a fertility rate over 2.0, the “replacement rate.”
This trend is fueled by a variety of socioeconomic and political factors. As inflation grows, the cost of living increases and the financial capacity to have kids declines. In the United States, nearly 60% of childless millennials have attributed their decision to delay having kids or forgo parenthood altogether to their inability to afford to raise children. Uncertainty about the political, economic, and environmental climate also serves as a deterrent.
But it’s not all bad news. Increasing access to healthcare — including contraceptives — means people are able to be more intentional about if and when they start a family. As women have more educational and employment opportunities, they have more options and may make decisions that result in them having fewer children.
As parental age increases, fertility rates decrease
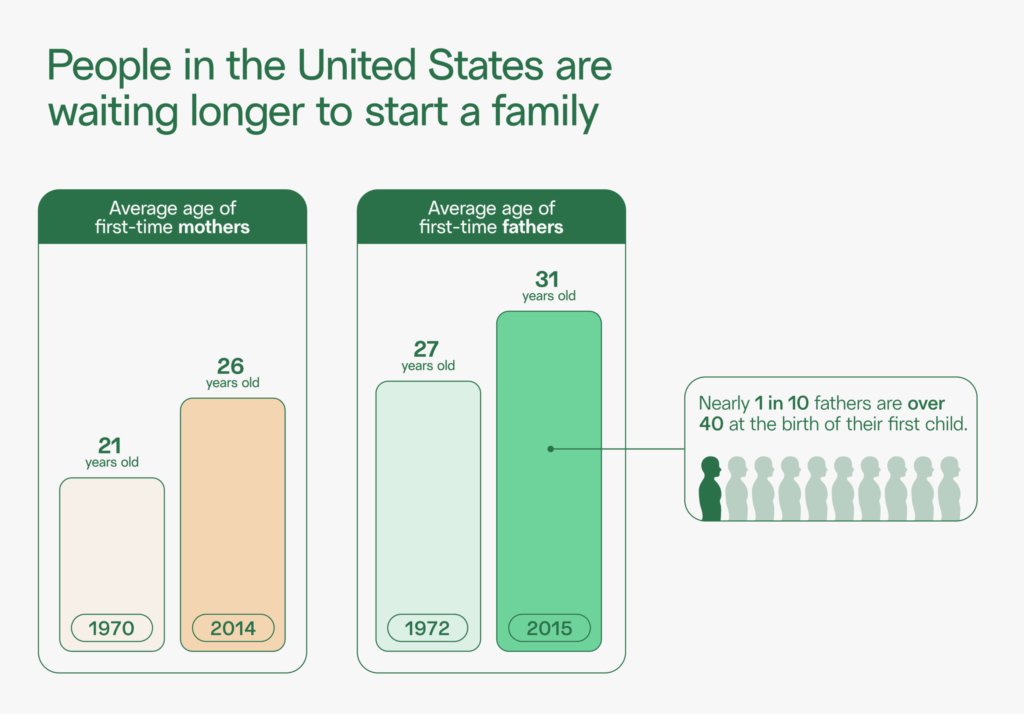
While these factors have led some to pursue a child-free lifestyle, others have just chosen to postpone when they have children. As parental age increases in high-income countries, like the US and the UK, more couples are likely to face infertility challenges.
In 1970, the average age of a first-time mother in the US was 21 years old. In 2014, the average increased to 26 years old. Paternal ages are also on the rise, with the average age of first-time fathers in the US increasing from 27 years old in 1972 to 31 years old in recent years. According to a 2017 study, nearly 1 in 10 fathers are over 40 at the birth of their first child.
In the UK, the average age of first-time parents has been steadily increasing since the 1970s. The average age of first-time mothers has risen from 26 to around 30; for fathers, the average age is 33.
Both partners’ ages are important fertility factors. Increased parental age is associated with increased chance of infertility, longer time to pregnancy, and fewer children, especially after age 35 for women and age 40 for men.
Sperm counts and quality in decline
The trends that we are observing extend beyond declining birth rates. It appears the scientific markers of male fertility, specifically sperm count and quality, may be dropping too.
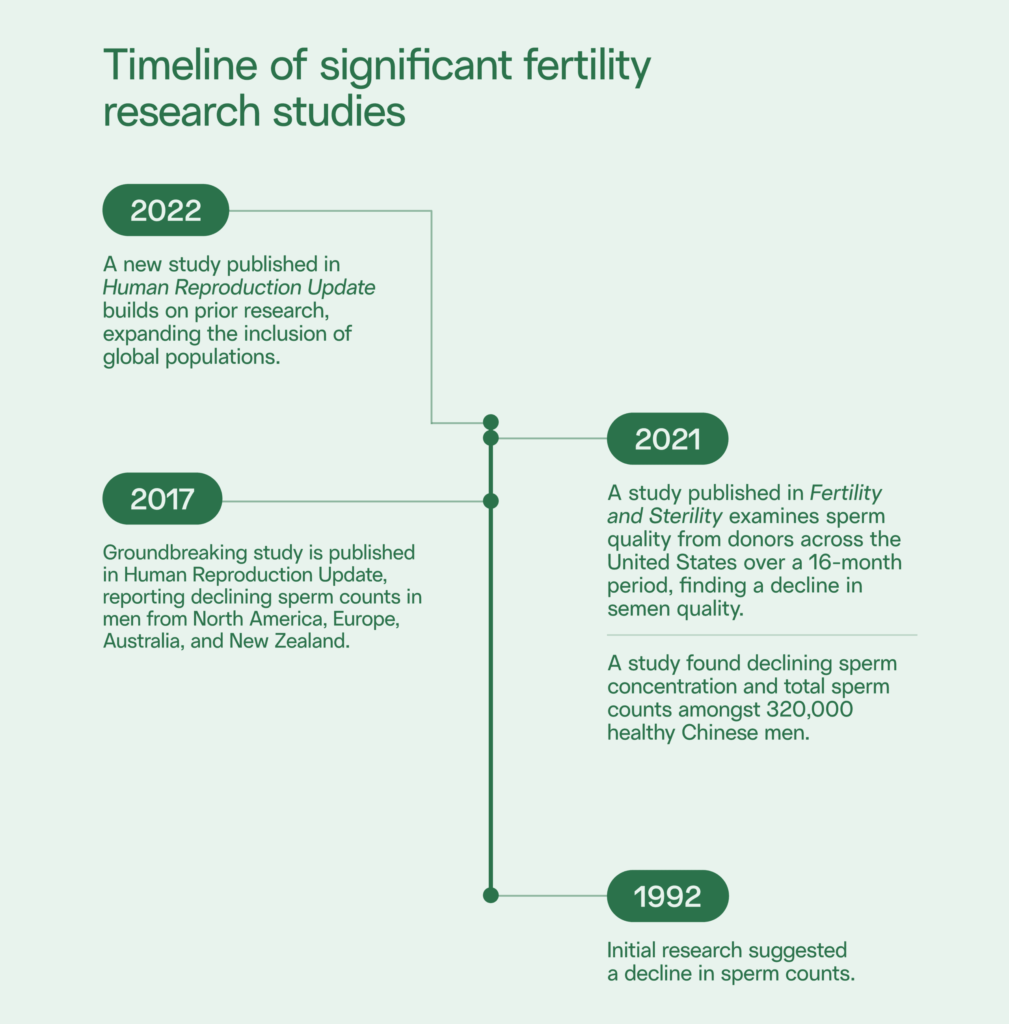
A 1992 study looking at over 50 years of semen analysis data — 61 studies of nearly 15,000 men — first introduced the idea of “spermageddon.” The results of the research found that average sperm concentration had declined by over 50%.
In 2017, one study that looked at changes in average sperm concentration between 1973 and 2011 gained public attention. The researchers aggregated sperm concentration data from 185 studies of 42,935 men. They found that sperm concentration had declined by 52.4%, and total sperm count dipped by 59.3%, in the time period studied.
This drop was significant and alarming enough to prompt the researchers to conclude that, due to the “significant public health implications of these results,” further research was “urgently needed.”
The same research team completed an update to their study in 2022, finding that not only were sperm counts still dropping — the decline was accelerating, and could be found globally.
In 2021, New York-based researchers completed another study of sperm count over time, this time looking at sperm donors in the United States (176,706 samples from 3,532 donors). Similarly, this study found a significant decline in average sperm concentration and motility (how well sperm are “swimming”) between 2005 and 2021.
Dr. Shanna Swan, researcher and author of Count Down, suggests that — if we follow the curve of the sperm count decline documented in the 2017 study — we’re on track to have an average sperm count of zero by 2045.
Controversy in research
But not everybody is sounding the alarm. There are some experts who are less convinced that we’re headed toward a full-blown crisis. Evaluations of the studies revealed that some of the research used in the 2017 meta-analysis was missing data points, like the men’s ages, which could explain the discrepancies in semen analysis results over time.
Some researchers argue that the natural variability of sperm counts could also explain some of the observed changes.
And even after dropping 52%, average sperm concentrations were still well within the normal range. In 2011, average sperm concentrations were just shy of 70 million sperm/mL of semen — above 15 million/mL, which is considered normal.
Finally, there have, of course, been changes and improvements in the way semen analysis is performed and reported since 1973. As one andrology expert noted, earlier scientists may have overcounted sperm.
Still — especially with the addition of the 2021 and 2022 studies indicating a continued decline over the past 16 years — there’s enough evidence to suggest that men are experiencing at least some reduction in sperm count and quality.

Possible causes of male fertility decline
So, why is this happening? The short answer: we don’t really know, and there needs to be more research. There are a number of possible hypotheses, but we’ve yet to pinpoint the exact cause for global male fertility decline.
Lifestyle: exercise, bodyweight, sleep
It’s no surprise that, in the Western world, our lives are more sedentary than ever before. Sedentary lifestyles have been shown to be negatively correlated with sperm health. Similarly, about two-thirds of the US and the UK are overweight or obese, a higher number than ever before; excess body weight is linked to lower semen parameters and reproductive hormone levels.
Declining sleep quality can also impact sperm production. Today, over 35% of working adults in the US don’t get enough sleep, up from 30% in 2010. Sleeping less than the recommended 7–8 hours per night has been correlated with lower markers of male fertility.
However, it’s unlikely that lifestyle factors alone can fully explain the global decline in sperm count. Household dogs are also experiencing a significant annual decline in average sperm count, indicating that environmental factors are at play too. Researchers found high concentrations of certain chemicals in the pets’ testes, further supporting this idea.
Chemical exposure
As Dr. Swan argues in Count Down, there’s some strong evidence that declining sperm count and overall fertility may be linked to our exposure to endocrine-disrupting chemicals (EDCs). EDCs are chemicals that interfere with the endocrine system and can be found in everyday plastics, pesticides, and household products.
Phthalates are a class of chemicals used to make plastic more flexible and durable. They are commonly found in vinyl flooring, carpeting, and personal care products. Dr. Swan’s research has concluded that phthalate exposure throughout a person’s life, through ingestion or skin contact, is associated with decreased semen parameters. (Phthalates were also what researchers found in the testes of the adult dogs they studied.)
Other EDCs include BPAs, often found in plastic water bottles; PFAS, used in non-stick cookware and firefighting foam; and glyphosate, the active ingredient in Round-Up and other pesticides. These and other endocrine disruptors have been repeatedly linked to lower sperm count and quality and increased DNA damage in sperm.
Legacy’s chief medical officer Dr. Ramy Abou Ghayda has also studied the impact of EDCs on sperm. His research has looked at the impact of exposure to organochlorine pesticides, associated with lower semen volume and sperm motility. He’s also studied the effects of bisphenol S (BPS), a common component in plastics, envelopes, boarding passes, glues, and many other everyday products. BPS is associated with poorer semen parameters, despite being marketed as a “safe” alternative to BPA.
Most people are exposed to these chemicals daily. Once endocrine disruptors enter the environment, they never completely break down, leading some researchers to call them “forever chemicals.” Plus, EDCs actually accumulate in fat and body tissues, so even if each individual exposure might be at a “safe” level, concentrations of these chemicals in our bodies can build up over time.
How can I protect my fertility?
Unfortunately, it is nearly impossible to avoid these chemicals completely as they are present everywhere — from food packaging to drinking water to soil. The best course of action is to remain conscious of items that increase your risk of exposure, to minimize the impact.
Steps to reduce your exposure to EDCs
- Avoid plastic and flame-retardant materials, especially in food packaging, children’s toys, furniture, and home flooring.
- Choose frozen, fresh, or dried foods over canned, as cans often contain BPA or BPS lining.
- Drink from the tap instead of bottled water (to reduce plastic exposure), and use a water filter to reduce EDCs in your drinking water.
- Check the ingredients of your household cleaning products and personal care items, and consider reducing how many of these you use on yourself and/or your kids.
While it’s good to eliminate the environmental exposures, switching to glass food containers and “clean” household products is just the first step. Many individuals can have significantly more control of their sperm quality and quantity by adjusting their health and lifestyle, including smoking cessation, weight loss, exercise, and supplementation with antioxidants. These efforts can even help counteract the negative impact of unavoidable environmental exposures.
To fully understand your sperm health, check out Legacy’s at-home male fertility testing.



