Guide to Sperm Testing
Sperm testing is the first step in understanding male fertility and provides a clear roadmap for sperm quality improvement. This guide will explain the essential sperm parameters that go into male fertility testing, what to expect during a semen analysis test, how to interpret the results, and what to do next to improve your sperm health.
Table of contents:
- Sperm basics
- Sperm parameters: count, motility, and morphology
- Male fertility testing: why check your sperm?
- Sperm testing process: what to expect when you’re doing a semen analysis
- How to read a semen analysis report
- Next steps: what to do with your sperm testing results
- References
Sperm basics
Before diving into the basics behind sperm testing and male fertility testing, it is important to gain a deeper understanding on the basics of sperm. This includes the components of sperm, as well as sperm parameters such as sperm count, sperm motility, and sperm morphology.
Components of sperm
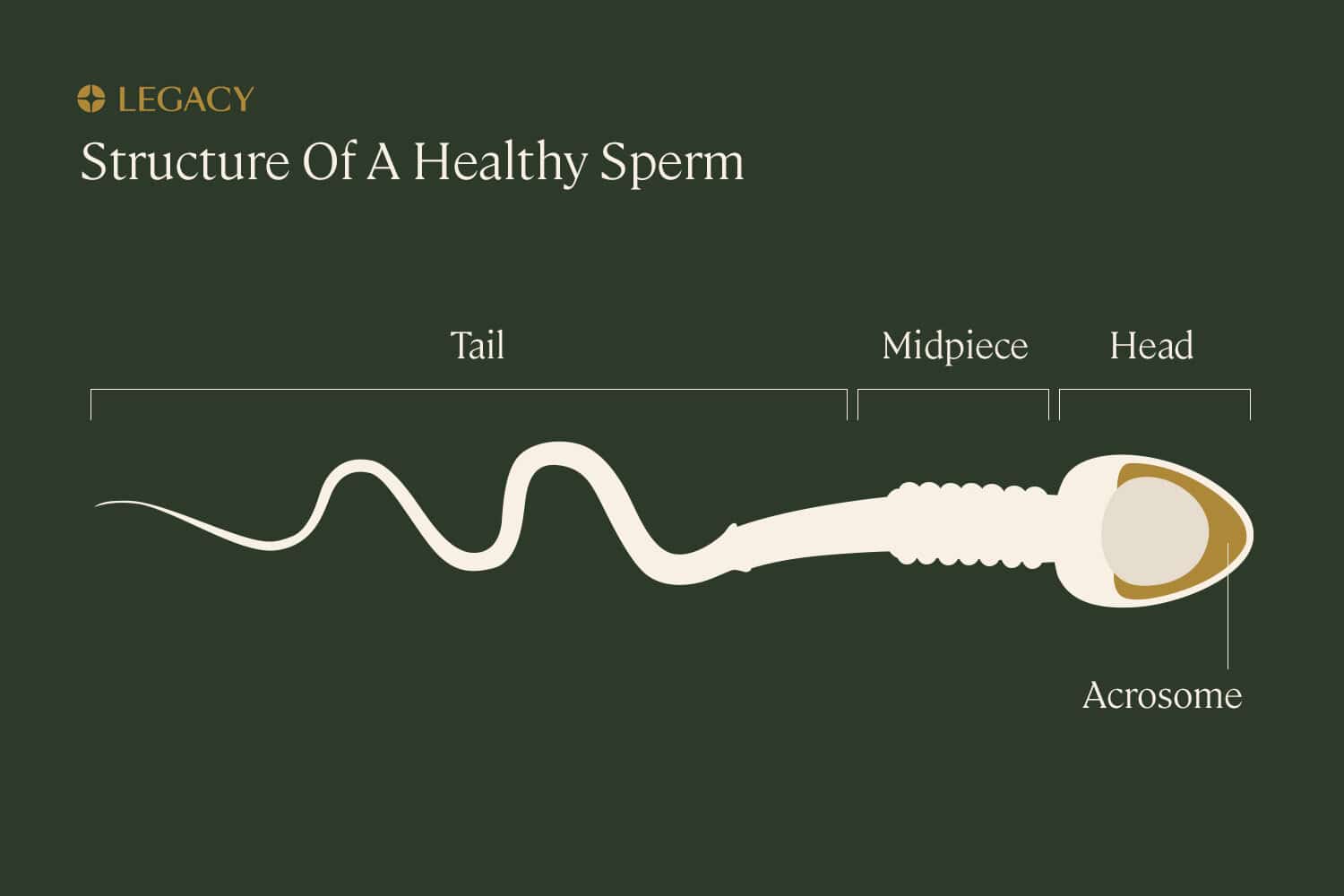
Sperm is the male sex cell, also known as a gamete. Sperm cells are composed of a few distinct parts:
- the tail, made of protein fibers, which helps it “swim” toward the egg
- the midpiece, or body/neck, which contains mitochondria to power the sperm’s movement
- the head, which houses the nucleus where the sperm’s precious cargo — genetic information — is stored, as well as the acrosome, a tiny structure at the tip of the sperm full of enzymes that helps the sperm penetrate the egg by digesting proteins and sugars on the surface of the egg.
A chromosome is a molecule of DNA, the material that guides the growth and development of the entire human body. Each sperm cell contains 23 chromosomes, which is half the number of chromosomes in a typical human cell. It’s known as a “haploid” cell. The egg contains the other half.
Together, they create a fully realized cell of 46 chromosomes (known as a “diploid” cell), which then divides to become all of the other cells in the body. The fact that half of our DNA comes from the sperm and the other half from the egg is why we inherit some traits from each of our parents.
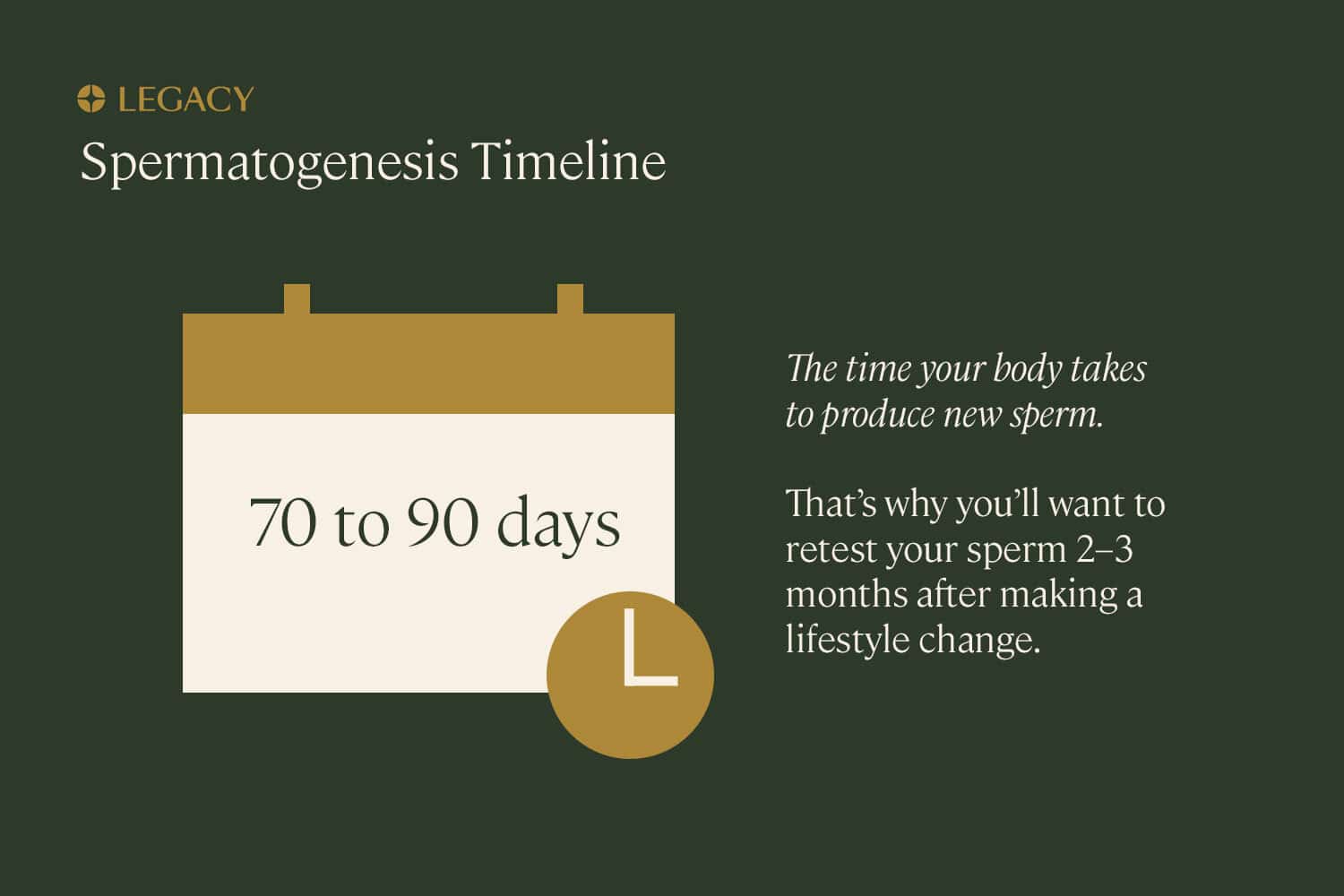
Sperm are produced in the testes (testicles) in a process called spermatogenesis, which takes about 74 days. Approximately 50–100 million viable sperm are produced by the testes each day. Spermatogenesis begins at puberty and continues, typically uninterrupted, until death. There are, however, changes in the health and quantity of the sperm with age.
Sperm parameters
There are several characteristics that, when examined in sperm testing, can indicate the health of sperm and overall male fertility.
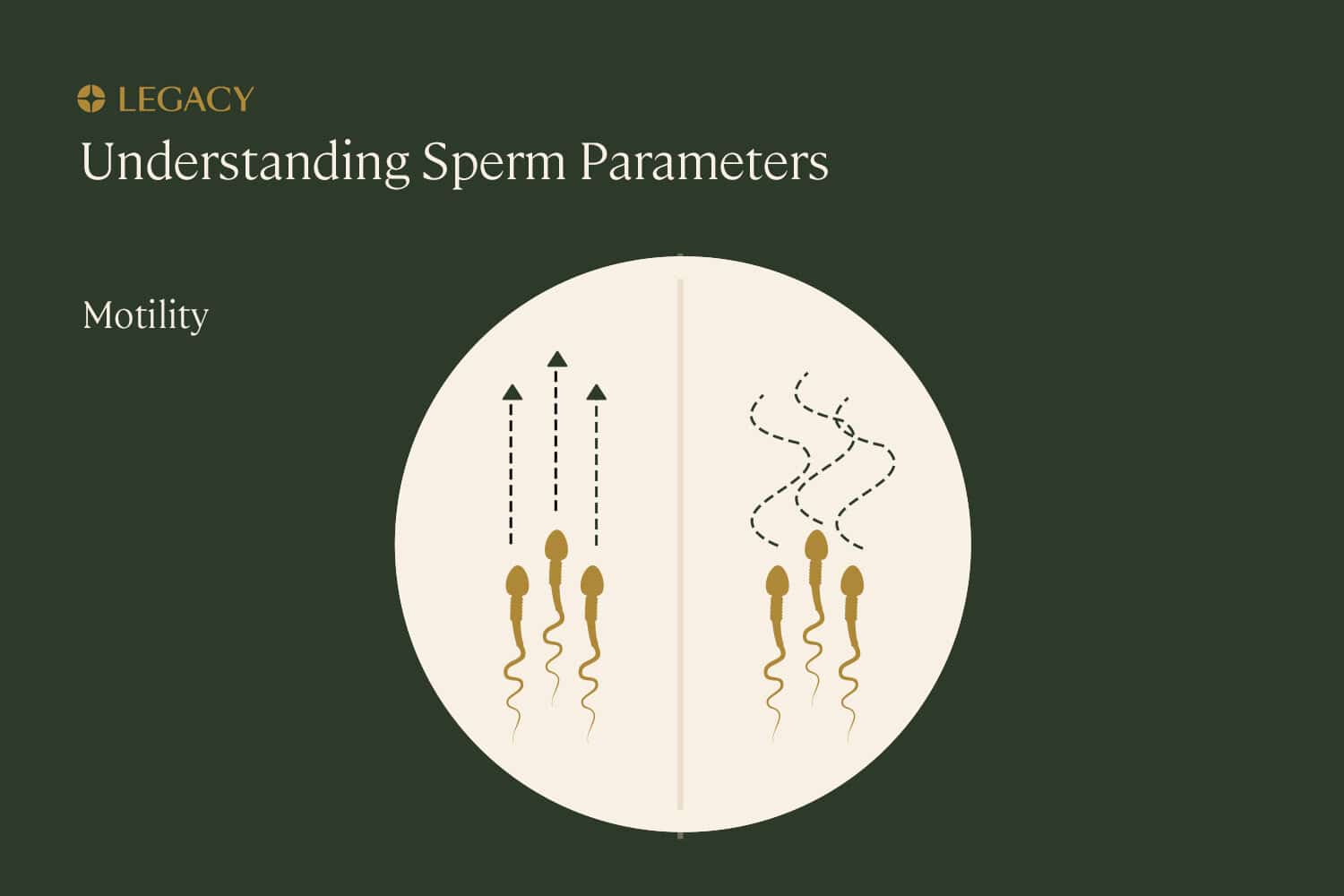
Sperm motility
Motility refers to the ability of the sperm to move or “swim,” which is essential for them to move through the female reproductive system and fertilize the egg. Progressive motility is the best type of movement that can be seen in sperm testing — that means the sperm is moving forward in straight lines or in large circles, as opposed to in small tight circles or along erratic paths.
Sperm count and concentration
Sperm count is the total number of sperm in a particular quantity of semen, the fluid that carries sperm out of the penis. Sperm concentration refers to how densely packed those sperm are within the semen.
For example, a sample may include 3 milliliters of semen (volume) and a concentration of 15 million sperm per mL. That would be a total sperm count of 45 million. Sperm testing will give you an accurate overview of these factors.
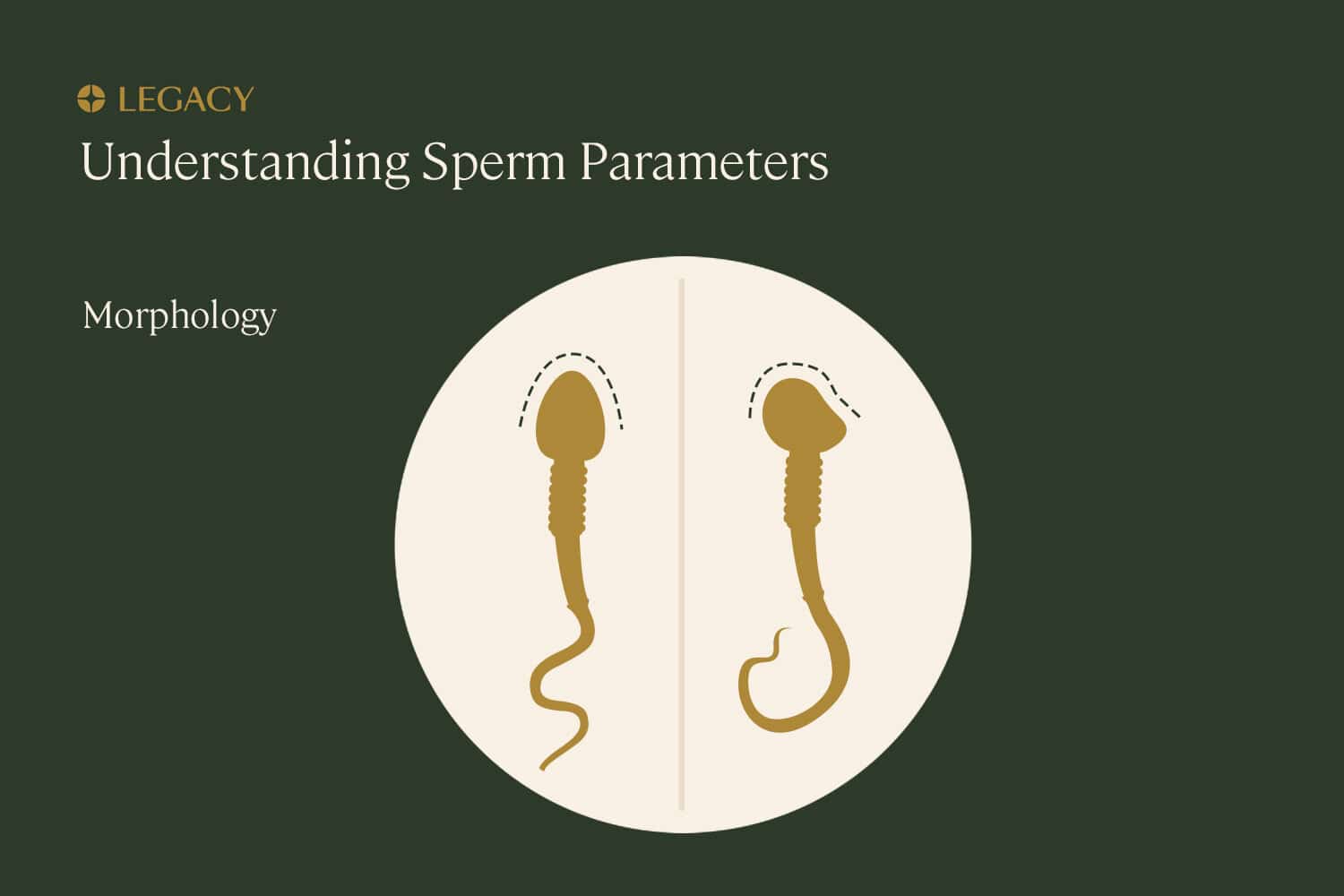
Sperm morphology
Morphology means the sperm’s structure or shape, which is ideally:
- a smooth oval head
- a well-defined acrosome, or cap, that covers 40–70% of the head
- a long tail with no visible abnormalities
This shape is important because it impacts a sperm’s ability to travel to and penetrate an egg. This is another factor revealed in some sperm testing. (Not every semen analysis looks at sperm morphology, but complete, clinic-grade analyses will include this measure.)
Male fertility testing
Male fertility testing is a set of tools used to estimate the chance that you’ll be able to achieve pregnancy. The best male fertility test we have is a semen analysis. A semen analysis tests for the health and fertility of sperm as well as the volume and chemistry of the semen, the fluid that carries sperm.
Legacy’s sperm testing kits are a great way to test male fertility at home and gain an up-to-date overview of your fertility and sperm health.
Why check the fertility of sperm?
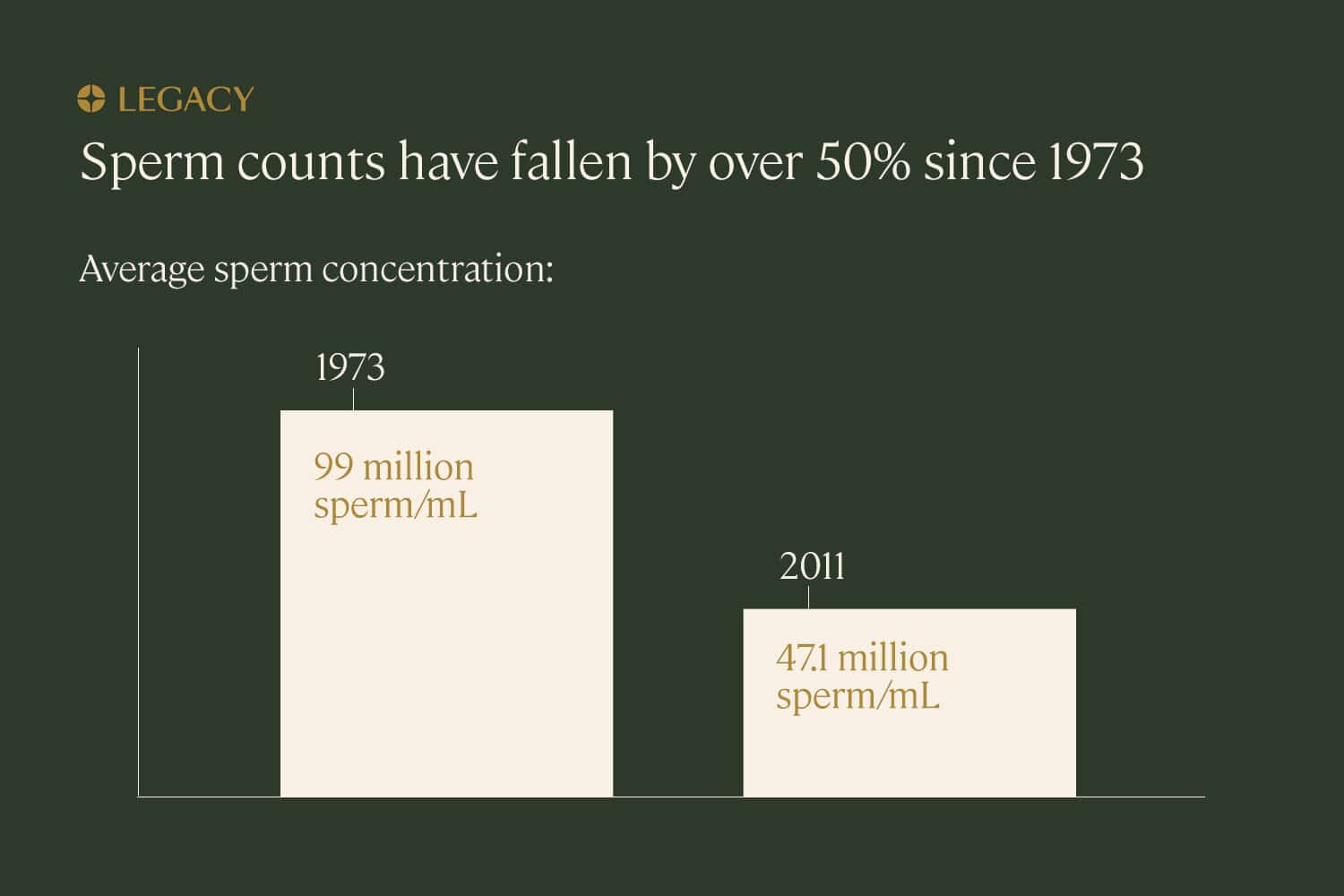
Male fertility issues contribute to 30–50% of diagnosed infertility cases. In the past four decades, sperm counts have dropped about 50%. Additionally, people are having children later in life than ever before, and age has an impact on male fertility: every 8 months of a male-bodied person’s life introduces a new genetic mutation into their sperm.
Learn more about age and male fertility and how male fertility testing can help identify sperm quality.
Sperm are a key component of male fertility. Without at least some healthy sperm, you won’t be able to create a healthy pregnancy without medical intervention.
Sperm testing is often done:
- If you are trying
to conceive. If you and your partner have been having unprotected sex for 6–12
months and haven’t yet gotten pregnant, semen analysis is a first-line test to help
diagnosis or rule out male fertility issues. Doing sperm testing and male fertility testing
early on in the process of trying to conceive can help you avoid costly and unnecessary
tests or treatments down the line.
- To proactively improve fertility.
Even if you’re not trying to conceive right now, you may want to proactively assess — and
address — sperm health issues. Because sperm take about 74 days to produce, it will take at
least 2–3 months for any lifestyle changes you make to have a measurable impact on your
sperm health. Sperm testing in advance can help ensure that, by the time you’re ready to
start a family, your sperm is in its best possible shape.
- If you plan to freeze your sperm.
If you’re freezing your sperm for the future—whether because you’re about to undergo cancer
treatment or because you simply want to preserve your sperm at its youngest, healthiest
state — sperm testing is crucial. You’ll want to ensure your sperm is healthy and fertile
before sperm freezing.
- To assess the results of a vasectomy or vasectomy reversal. If you have a vasectomy for long-term birth control, it’s recommended that you get a semen analysis around 12 weeks after the procedure, to confirm the vasectomy has worked as intended. Similarly, if you have surgery to reverse a previous vasectomy, sperm testing every month for 12 months is recommended to ensure sperm quality, count, and motility is recovering normally.
Learn more about why semen testing is important.
Sperm testing: What to expect
How is sperm testing done? And which is the best sperm count test for you — in-office, or at-home?
In-office semen analysis
Traditionally, a semen analysis happens at a fertility clinic or urologist’s office with an andrology lab (a lab specifically set up for sperm testing, processing, and freezing). In this context, the office will usually require a prescription or referral from your doctor.
The semen sample for sperm testing is typically collected in a small cup via masturbation, either there in the office (in a “collection room”) or at home, and brought to the lab within 60 minutes. From there, the lab staff will examine the sample under a microscope to evaluate the sperm count, morphology, and motility, and results will be prepared and available in a few days.
At-home semen analysis
With at-home sperm analysis, such as what’s offered here at Legacy, you are able to collect your sample in the comfort of your home. The Legacy sperm testing kit includes a special buffering medium that keeps your sample viable for up to 48 hours, as opposed to the usual 60 minutes. The sample is shipped overnight to the lab, where a technician will analyze it.
Many mail-in and at-home sperm testing kits give only the basic results, like sperm count and concentration. Legacy’s at-home sperm testing kits tests for every sperm parameter evaluated in an andrology lab, and offers personalized recommendations for improving sperm health based on your lifestyle and sperm testing results.
Semen analysis cost
A typical cost for an in-office semen analysis is about $250, but it requires a prescription from a doctor, and the office visit will have a separate fee. The cost of a Legacy at-home semen analysis is $375, and it does not require a prescription from a doctor. Our at-home sperm testing kits can be delivered to your home in as little as two business days.

Important sperm testing tips:
- How long to abstain before sperm testing?
Sperm counts are highest if you’ve waited at least 2 days between
instances of ejaculation, but waiting
longer than 5 days can mean your sample will have fewer motile sperm and
lower sperm quality. So, for
best results, you should abstain from ejaculation for 2–5 days before producing your
sample for sperm testing.
- Personal lubricant and even saliva can
impact the results of your sperm testing. Special fertility-friendly lube, like
Pre-Seed, is an alternative that’s been shown to have little
impact on semen analysis results. Still, we recommend using no lube or
saliva for the most accurate semen analysis results.
- It may sound obvious, but a sperm testing
sample shouldn’t be collected in a condom. Many condoms contain spermicidal
ingredients.
- Sperm health can be affected by illness and fever, so try to avoid doing sperm testing when you’re sick or recovering from sickness.
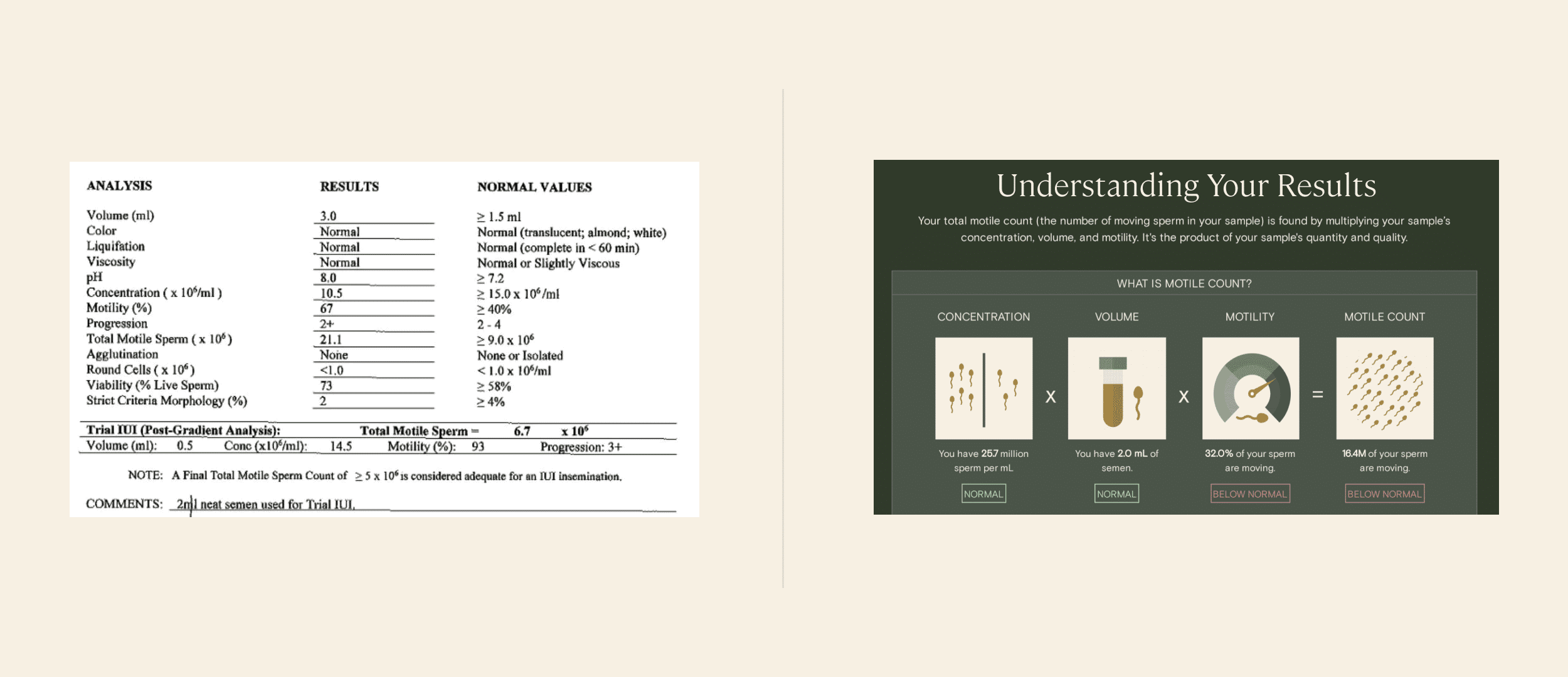
A typical semen analysis report vs. just one page of Legacy’s in-depth, patient-friendly report. See a full sample Legacy semen analysis report.
How to read a semen analysis report
Your semen analysis report will include a variety of values. Here’s an overview of what your sperm testing results mean.
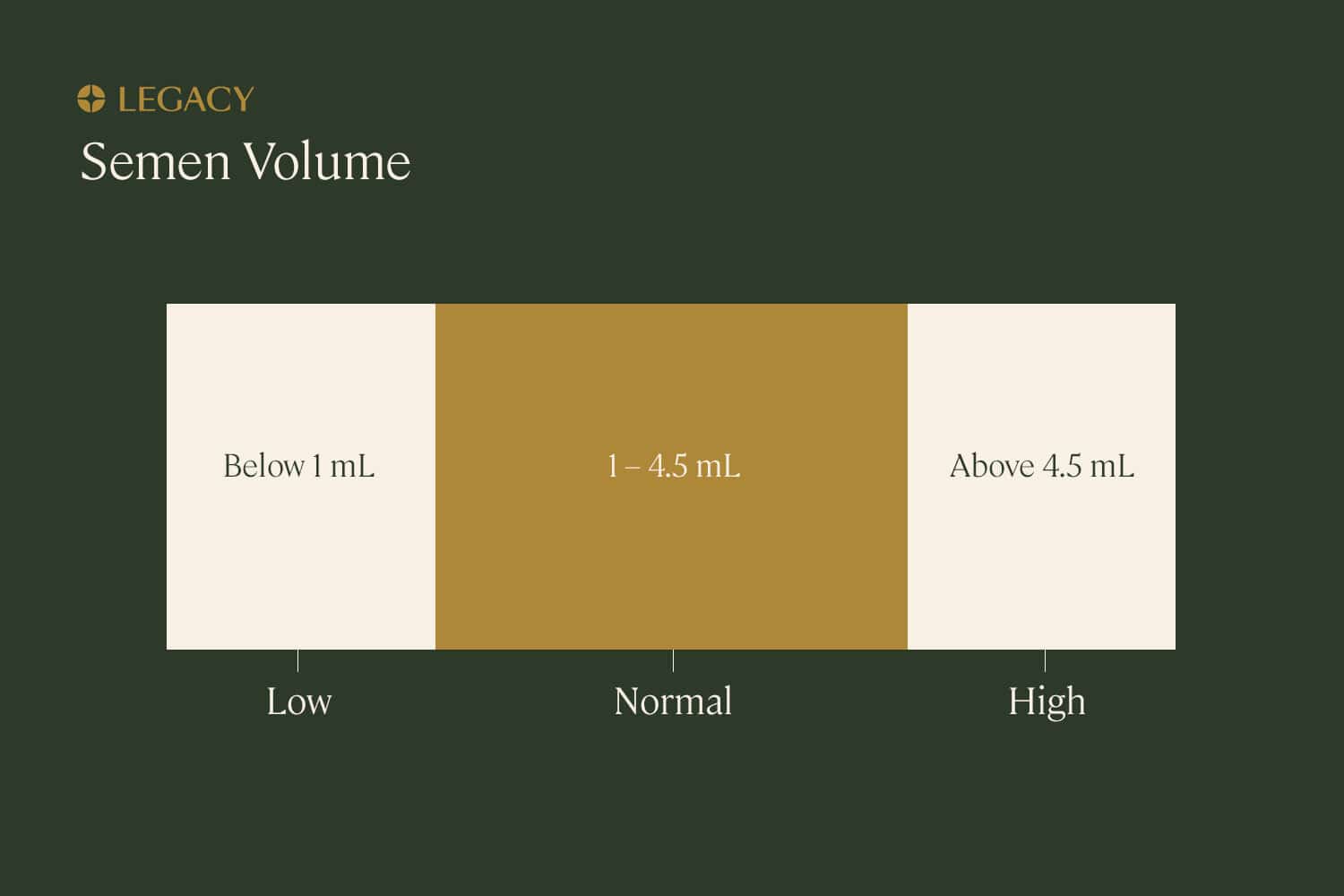
Semen volume
Semen volume refers to the volume of the entire sample sent to the lab. A normal semen volume is 1.5 mL to 4.5 mL; lower than 1.5mL is considered “low” and higher than 4.5mL is considered “high.”
A low semen volume, known as hypospermia, could be caused by a variety of structural issues in or illnesses of the male reproductive system, and can contribute to subfertility. Our at-home sperm testing kits will quickly highlight this.
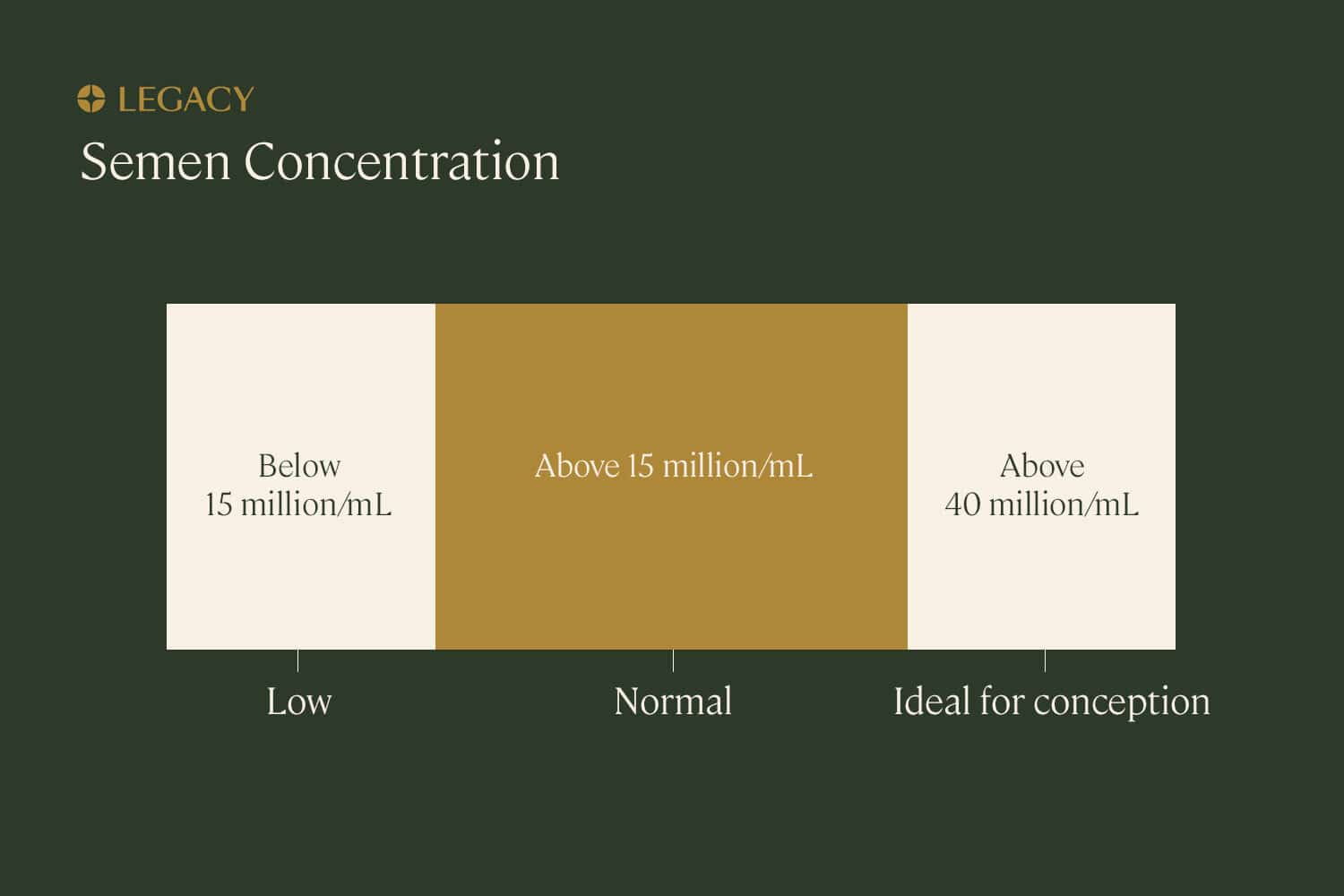
Sperm concentration
Fifteen million sperm per milliliter of semen is considered a normal sperm concentration, but researchers have noted that concentrations under 40 million/mL may impede chances of pregnancy.
Having too little sperm in your semen is known as oligospermia; having no sperm at all is known as azoospermia. Both conditions can contribute to infertility. You can be alerted to these conditions with at-home sperm testing kits or male fertility testing.
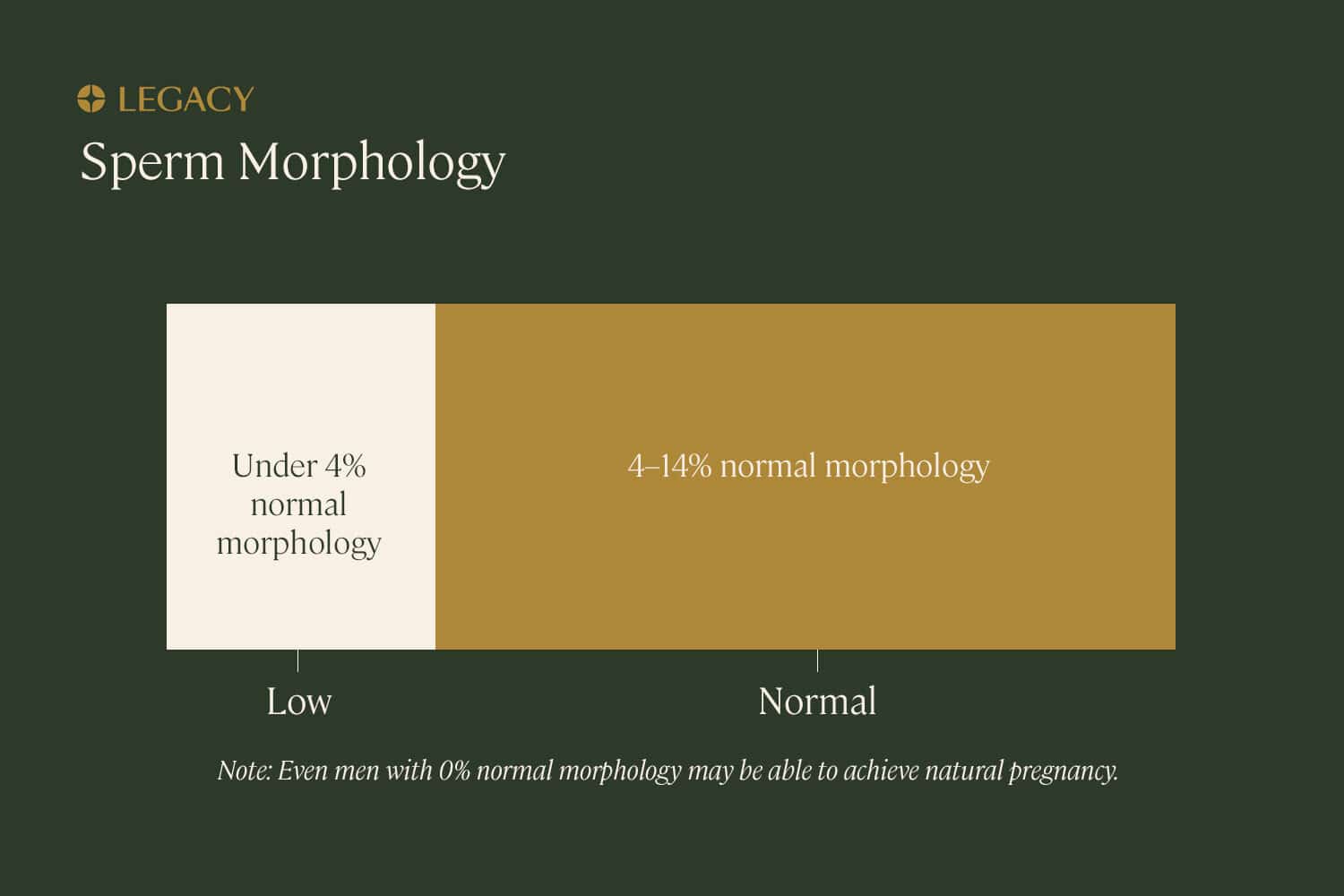
Sperm morphology details
Morphology refers to the proper shape and structure of sperm, which is essential for it to move toward and fertilize an egg. Sperm morphology testing can be done using one of two sets of criteria:
- Kruger morphology criteria are very strict, and under this method of testing, very small discrepancies will deem sperm abnormal.
- World Health Organization (WHO) sperm testing is slightly more lenient, with a wider range of “normal” morphology.
- Your sperm testing results will report the percentage of “normal forms.” Every sample will have some abnormal sperm. In fact, a healthy sperm morphology result may be as few as 4–14% normal sperm, depending on the criteria.
Abnormal sperm can come in a multitude of forms. In some reports, you may see a breakdown of the types of abnormal sperm your sample contains. Some examples include:
- Abnormalities in the sperm head size or shape, including amorphous, pyriform, vacuolated, tapering, or large heads.
- Defects in the sperm midpiece or “neck,” including a bent or asymmetrical neck.
- Defects or absence of the acrosome, the cap that covers the sperm head and helps the sperm penetrate the egg.
- Abnormalities in the sperm tail, such as a coiled tail.
- Multiple heads or tails, or the absence of heads or tails.
- The presence of droplets of excess residual cytoplasm, or cell material that once held immature sperm together but should have been removed during the maturation process.
Poor sperm morphology, as evidenced by a low percentage of normal sperm, is known as teratozoospermia. It’s important to note that a very low percentage of normal sperm — or even no normally shaped sperm at all — does not necessarily mean you are infertile.
In one study, nearly 30% of men with 0% normal morphology were still able to achieve pregnancy with their partner without fertility treatment, as compared to 55% of men with healthy morphology results. Morphology is just one of many factors that contribute to the overall understanding of male fertility.
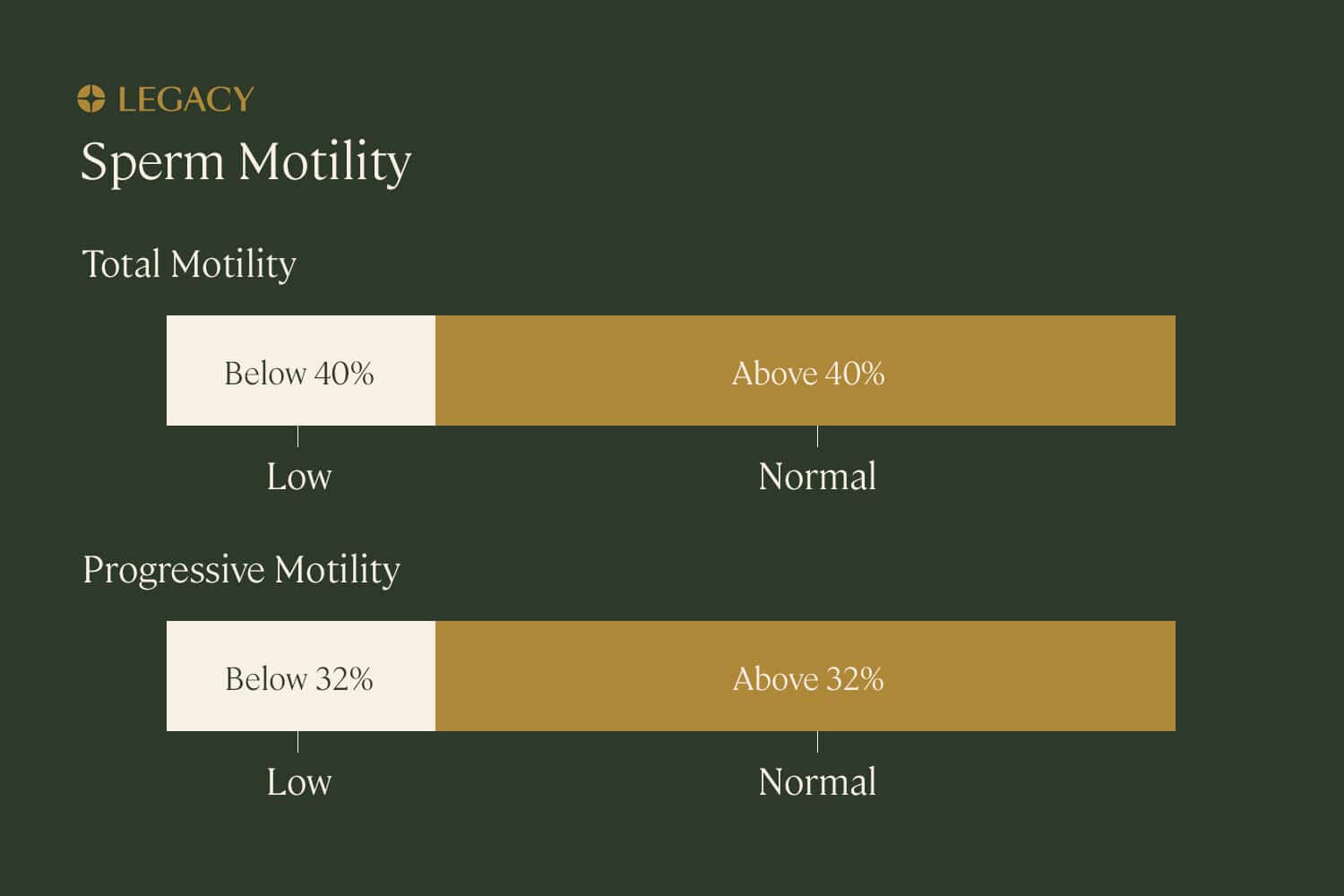
Sperm motility details
As part of your at-home sperm testing results, you’ll get details on your sperm motility test results. The first value you’ll get is total motility, which is the percentage of your sperm that are in motion; ideally, 40–50% of your sperm are motile.
The report will also include progressive motility, the percentage of your sperm that are not just motile, but moving in a helpful manner — in straight lines or in large circles.
Non-motile sperm may be slow, sluggish, or completely immobile (not moving at all). Poor sperm motility or asthenospermia is diagnosed when less than 32% of the sperm are able to move efficiently.
On more comprehensive sperm testing results, you may also get a few other parameters, such as:
- Velocity (speed).
- Amplitude of lateral head displacement (ALH), a measure of how much the head of the sperm rotates or moves from side to side.
- Linearity, a measurement of how quickly the sperm moves on its forward path (as opposed to just how quickly it moves from side to side or in circles).
- Beat cross frequency, or how often the head of the sperm moves across the middle of its path.
Each of these sperm testing values help lab technicians determine total and progressive motility.
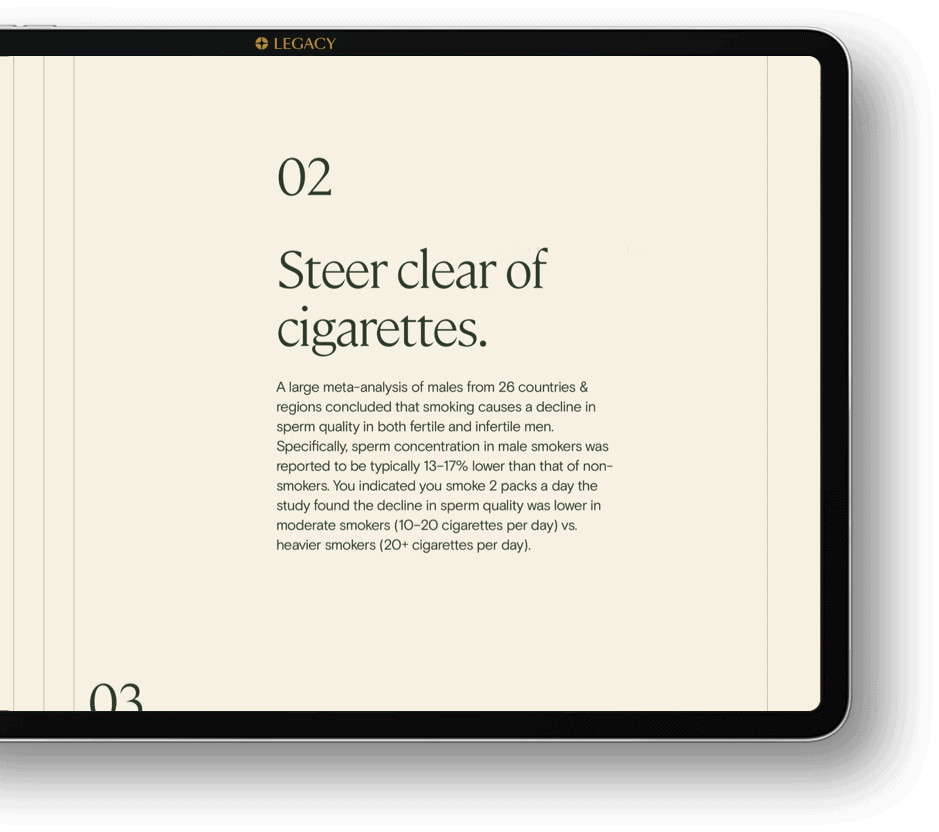
Personalized recommendations
Legacy’s at-home sperm testing kits include a unique benefit: guidance on how to improve your sperm health, based on questions you’ve answered about your lifestyle (for example, how often you exercise, your diet, and the type of underwear you wear).
These recommendations can help you understand how your lifestyle choices impact your sperm health and sperm testing results, and how to make changes that will result in healthier sperm and higher fertility.
Next steps after a semen analysis
Once you have completed a semen analysis, you might be asking yourself, what’s next? Male fertility testing and at-home sperm testing should help provide you with a clear path forward on the way to sperm quality improvement.
Improving your sperm count, motility, or morphology naturally
If you’ve received sperm testing results with low sperm count/concentration or poor motility or morphology, there are some things you can do on your own to improve these parameters. Your Legacy report will include personalized recommendations for improving your sperm health, based on your lifestyle. Optimizing your diet, increasing how much you exercise, quitting smoking, and cutting back on alcohol are all examples of ways to naturally improve your sperm health.
When to retest with another semen analysis
Whether or not, and when, you should redo sperm testing depends on why you’re testing in the first place. If you’ve received a completely normal result, you may not need or want to repeat sperm testing at this time.
If you’ve received an abnormal sperm testing result that you believe is due to a spilled or contaminated sample, a too-short period of abstinence prior to the test, illness or fever at the time of the test, or some other anomaly, you can retest again after 2–5 days of abstinence from ejaculation.
For those who have had a vasectomy, you should test your sperm approximately 12 weeks after the surgery to ensure it was successful. For those who are doing sperm testing after a vasectomy reversal, the recommended frequency is to retest once per month for 12 months, to ensure that sperm count and quality are recovering as they should.
For those who are making lifestyle changes and hope to see improvements in their sperm testing results, it’s important to know that sperm take about 74 days to produce through the process of spermatogenesis. Therefore, any changes will take at least 2–3 months to affect your sperm testing results. If you’ve, for example, quit smoking or started an exercise routine, you may want to retest again 3 months later to see how that change has improved your fertility health.
When to see a specialist for male infertility
If you have received a very abnormal semen analysis report (for example, no sperm was found at all), you’ve attempted to make lifestyle changes with no impact on your sperm testing results, or you have not been able to achieve pregnancy with your partner after 6–12 months of unprotected sex, it’s recommended that you see a doctor for a consultation.
You might see a reproductive endocrinologist (who sees couples trying to conceive) or a urologist (who treats male patients for infertility and sexual health dysfunction). Be sure to bring your semen analysis results to your appointment to discuss with your doctor.

Sperm freezing after semen analysis
If your at-home sperm testing results demonstrate you have healthy, fertile sperm, and you’re not planning to start a family right now, you should consider sperm freezing.
Sperm freezing ensures that your healthy sperm can be used in the years to come, as your natural fertility decreases. It also preserves your parenthood options in the event that an illness or accident threatens your fertility. Scientific research tells us that sperm can be frozen indefinitely with no loss in quality.
Learn more about sperm freezing.
References
- C.H. Heller, Y. Clermont. “Kinetics of the germinal epithelium in man.” Recent Progress in Hormone Research, 1964.
- Isiah D. Harris, MD et al. “Fertility and the Aging Male.” Reviews in Urology, 2011.
- Vanessa A. Comar et al. “Influence of the abstinence period on human sperm quality: analysis of 2,458 semen samples.” JBRA Assisted Reproduction, 2017.
- Ashok Agarwal et al. “Abstinence Time and Its Impact on Basic and Advanced Semen Parameters.” Urology, 2016.
- Ashok Agarwal et al. “Effect of an isotonic lubricant on sperm collection and sperm quality.” Fertility & Sterility, 2013.
- Elisabeth Carlsen et al. “History of febrile illness and variation in semen quality.” Human Reproduction, 2003.
- K. Gopalkrishnan et al. “Volume of semen as a parameter of its quality.” Indian Journal of Medical Research, 1992.
- Matthew Roberts, MD and Keith Jarvi, MD. “Steps in the investigation and management of low semen volume in the infertile man.” Canadian Urological Association Journal, 2009.
- Trevor G. Cooper et al. “World Health Organization reference values for human semen characteristics.” Human Reproduction Update, 2009.
- Niels E. Skakkebaek. “Normal reference ranges for semen quality and their relations to fecundity.” Asian Journal of Andrology, 2010.
- Roelof Menkveld. “Clinical significance of the low normal sperm morphology value as proposed in the fifth edition of the WHO Laboratory Manual for the Examination and Processing of Human Semen.” Asian Journal of Andrology, 2010.
- Jason R. Kovac et al. “Men with a complete absence of normal sperm morphology exhibit high rates of success without assisted reproduction.” Asian Journal of Andrology, 2017.
- Hagai Levine et al. “Temporal trends in sperm count: a systematic review and meta-regression analysis.” Human Reproduction Update, 2017.
- Augustine Kong et al. “Rate of de novo mutations, father’s age, and disease risk.” Nature, 2012.