Guide to Sperm Improvement
When it comes to sperm improvement and male fertility improvement, there’s a lot you can do on your own. What exactly is sperm improvement? This typically includes a combination of the following: sperm quality improvement, sperm morphology improvement, sperm count improvement, and sperm motility improvement.
Simple lifestyle changes have been positively correlated with sperm health and sperm quality improvement. This guide will explain the research behind sperm improvement, and provide some steps you can take on the path to male fertility improvement and increasing male fertility.
Table of contents:

Understanding sperm parameters
There are several characteristics that can indicate the health of sperm, and are closely associated with overall male fertility improvement. Understanding which sperm improvements will benefit you starts with understanding these characteristics of male fertility. Normal values (below) according to the World Health Organization’s 5th Edition.

Sperm count/concentration
Sperm count is the total number of sperm in the entire semen sample (one ejaculation). Sperm concentration refers to the number of sperm per unit volume (milliliter) of semen. For example, a sample may include 3 milliliters of semen and a total sperm count of 45 million; that would be a concentration of 15 million sperm per mL.
Normal values: At least 15 million sperm/mL of semen.
Possible issues: Having too little sperm in your semen is known as oligospermia; having no sperm at all is known as azoospermia. These can both contribute to male-factor infertility.
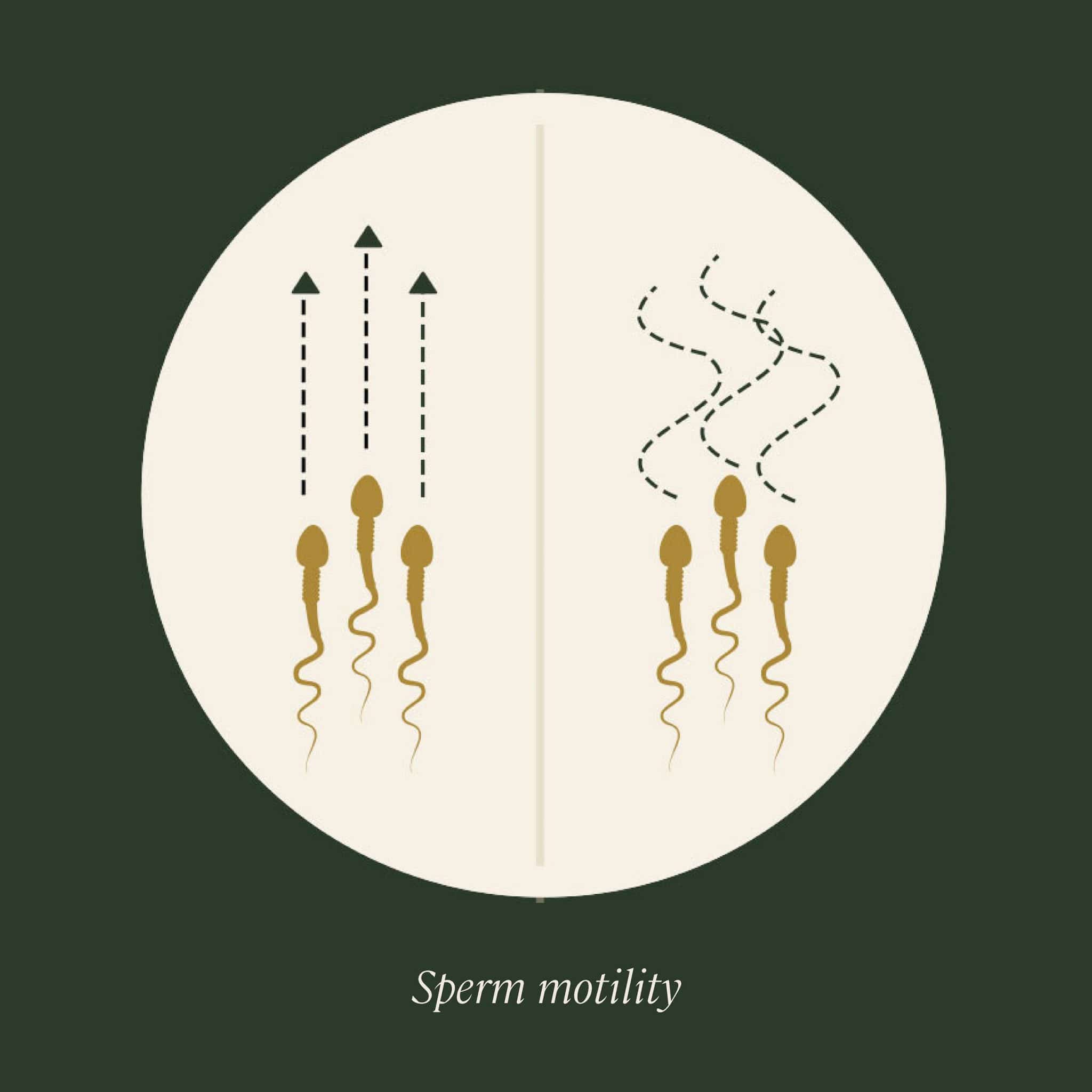
Sperm motility
Motility refers to the ability of the sperm to move or “swim” through the female reproductive system, which is essential to reach and fertilize the egg and is another crucial sperm quality parameter. Progressive motility means the sperm move forward in straight lines or in large circles, as opposed to in tight circles or along erratic paths.
Normal values: Motile sperm, at least 40%; progressively motile sperm, at least 32%.
Possible issues: Poor sperm motility, diagnosed when there’s a low percentage of motile sperm, is known as asthenospermia/asthenozoospermia. This is one of the most common male-factor infertility issues. However, sperm motility improvement can be accomplished with male fertility supplements and lifestyle changes.

Sperm morphology
Morphology means the sperm’s structure or shape, which is ideally a smooth oval head; a well-defined acrosome, or cap, that covers 40–70% of the head; and a long tail with no visible abnormalities. This shape is an important factor in sperm quality because it impacts a sperm’s ability to travel to and fertilize to the egg. Sperm morphology can be assessed using either the stricter Kruger criteria, or using the World Health Organization (WHO) criteria, which is more lenient.
Normal values: At least 4% normal forms
Possible issues: Poor sperm morphology, as evidenced by a low percentage of normal sperm, is another common male-factor infertility issue known as teratozoospermia. Lifestyle changes, such as quitting smoking and reducing drinking, can lead to overall sperm quality improvement and sperm morphology improvement.
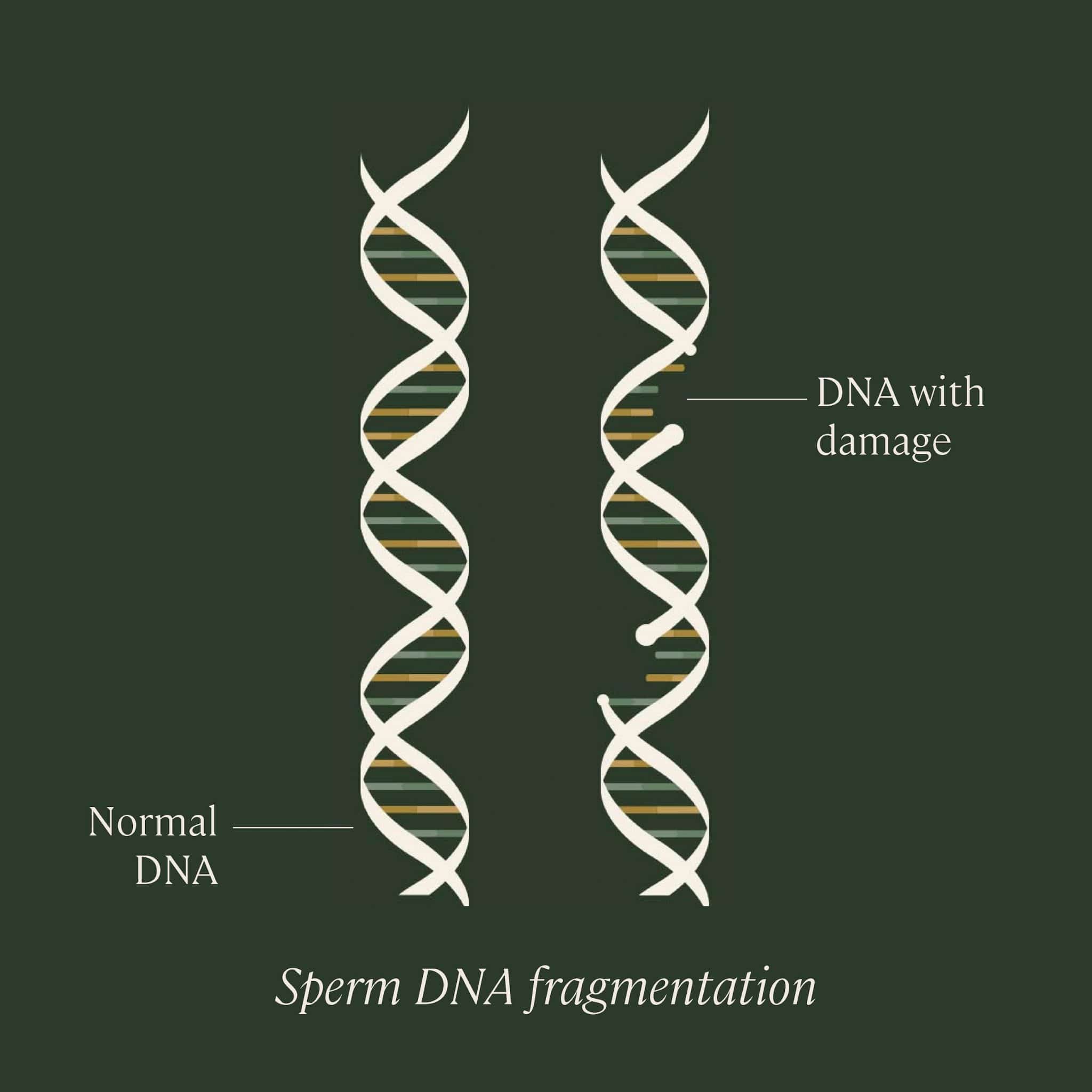
Sperm DNA fragmentation
DNA fragmentation refers to the degree of damage to the genetic material carried by sperm, such as separation or breaking of DNA strands into pieces. If the sperm contains a lot of DNA that’s broken or unstable, it may be more difficult for it to fertilize an egg, or it may increase the chances of miscarriage or birth defects. Research is still ongoing in order to fully understand the effects of DNA fragmentation of fertilization and fertility.
Normal values of DNA fragmentation index (DFI): Depends on testing; usually the “normal” cutoff is 30% using the SCSA test. DNA fragmentation is not usually tested as part of a typical semen analysis, but can outline the best next steps towards sperm improvement and sperm quality improvement.
Learn more about sperm DNA fragmentation.
First step to male fertility improvement: sperm testing
The best way to test your sperm health, sperm quality and understand any sperm improvements you may need to make, is to do a semen analysis. This test involves providing a semen sample, collected via masturbation, to a lab. There, it will be examined under a microscope to determine your semen volume and sperm count, concentration, what percentage of your sperm are motile, and your ratio of properly formed sperm, known as morphology.
The test can be done in a fertility clinic or urologist’s office, or can be done from the comfort and privacy of home with a mail-in sperm testing kit, like we offer. The results of your semen analysis will tell you which of your sperm parameters are normal, and which (if any) are abnormal. The Legacy semen analysis report also includes personalized recommendations for sperm improvement, based on your lifestyle.
A semen analysis provides the foundation for overall sperm improvement and sperm quality improvement, including sperm motility improvement, sperm morphology improvement, and sperm motility improvement.
Learn more in our Guide to Sperm Testing.

Why is
sperm improvement important?
Sperm are a key component of fertility in cisgender men and other people with sperm. Without at least some healthy sperm, you most likely won’t be able to achieve pregnancy, and you might need medical intervention and/or assisted reproductive techniques (ART) such as intrauterine insemination (IUI) or in vitro fertilization (IVF) to treat male-factor infertility.
Some emerging research is illuminating the relationship between sperm health, natural conception rates, risk of miscarriage, and the success of ARTs.
Male-factor infertility is solely responsible for 20–30% of infertility cases, and contributes to up to 50% of overall cases. Some studies have reported a drop of sperm counts by up to 50% in the past four decades. Researchers have proposed that pollution, diet, lifestyle, or exposure to chemicals that disrupt the endocrine system, among many other factors, could be to blame for decreased sperm quality.
The good news is that you are creating millions of sperm every single day; it takes about 74 days on average for the process of spermatogenesis to go from stem cell to final, mature sperm cell. So, if you make positive lifestyle changes, you could see sperm quality improvement within a few months.

What impacts male fertility, and what changes can I make to improve my sperm health?
Male fertility improvement and sperm quality improvement can be achieved by lifestyle choices, including quitting smoking, reducing drinking, and striking a balanced diet. These subtle changes may lead to sperm count improvement, sperm morphology improvement, and sperm motility improvement among other notable differences.
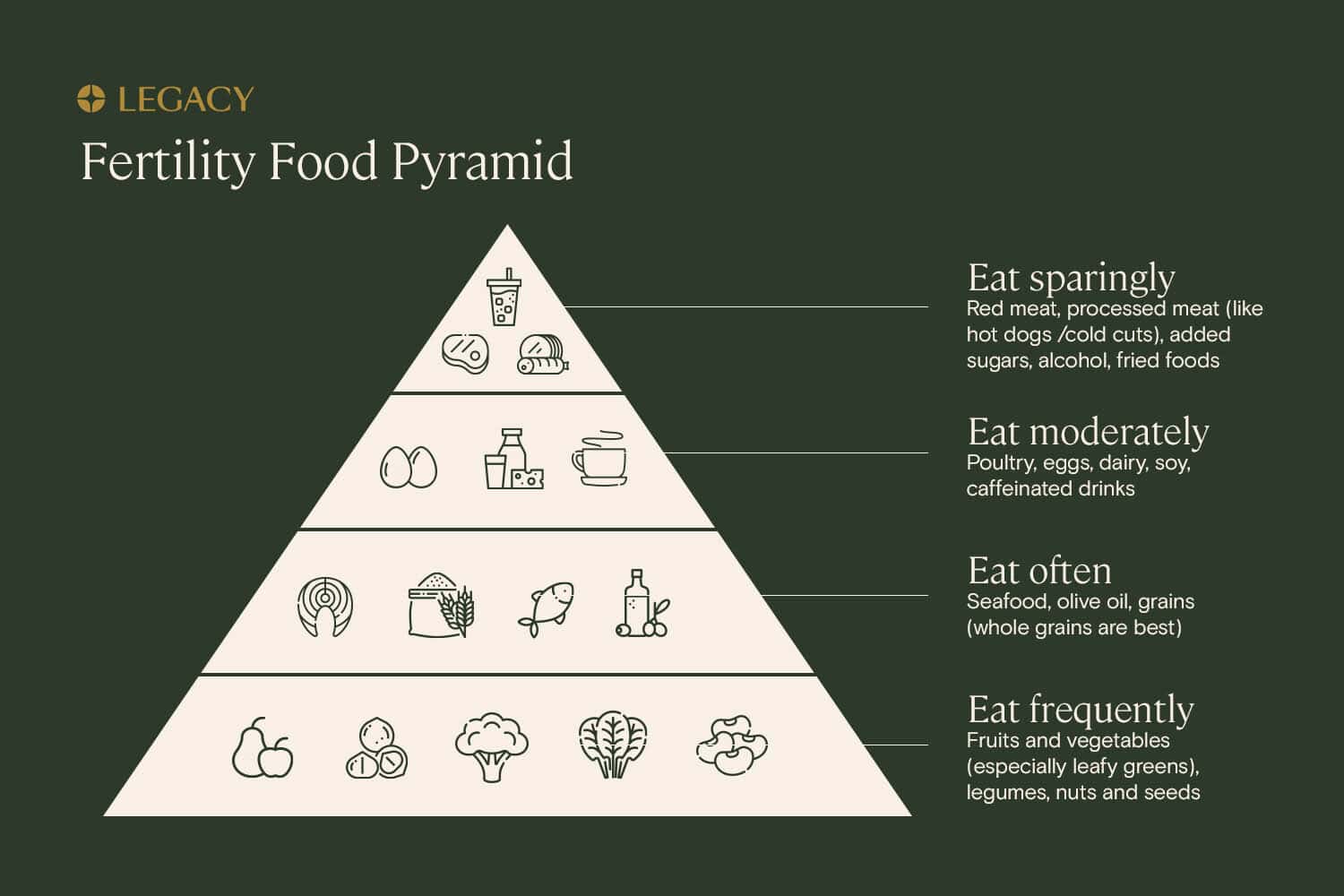
Diet and sperm health
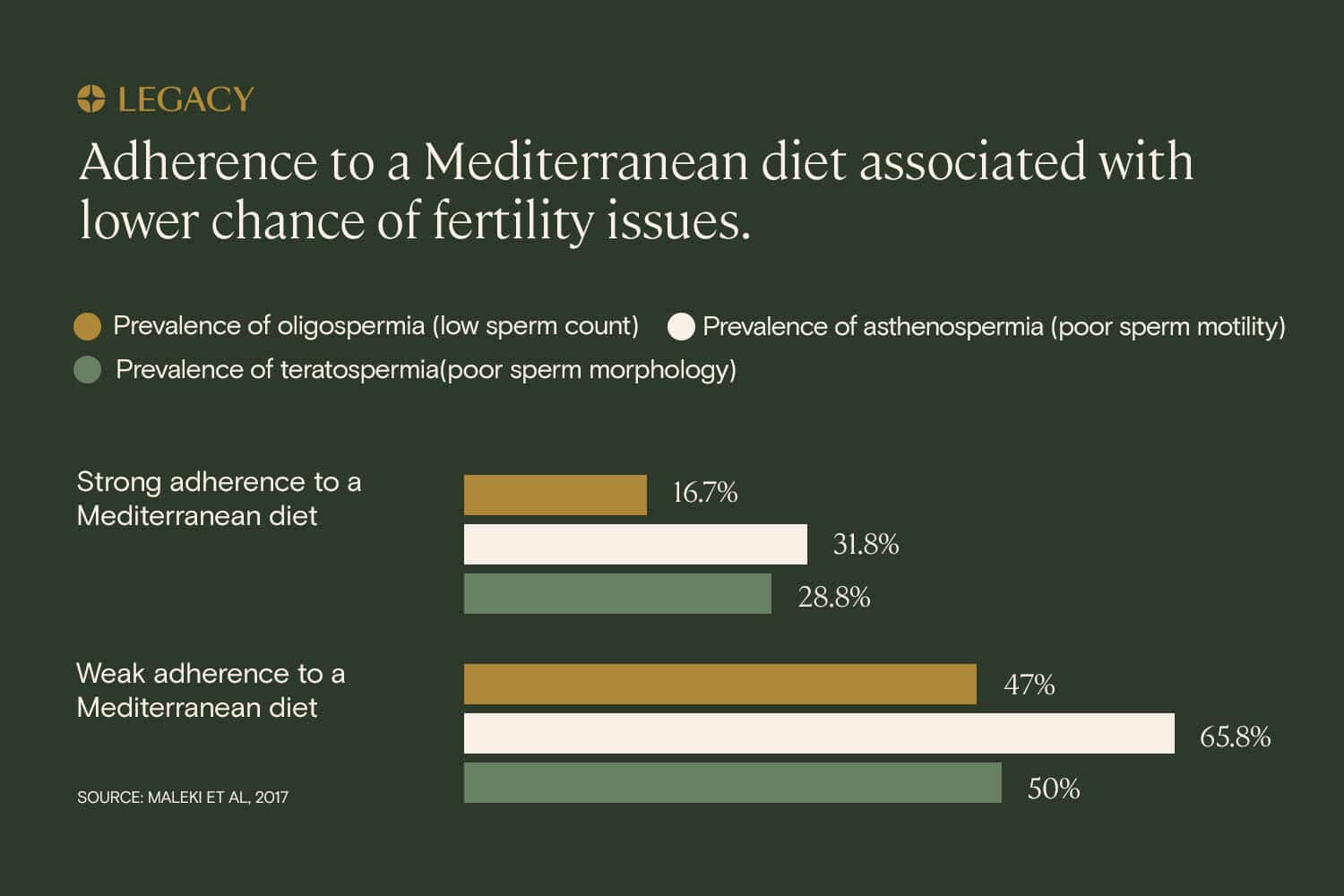
Studying the impact of diet on male fertility is a complex process, and is still not fully elucidated. The difficulty of evaluating the exact composition of a person’s diet and accounting for all possible variables has resulted in a scarcity of strong evidence about how nutrition affects sperm health and sperm quality. However, the available data show that certain dietary patterns can be associated with worse or better semen parameters.
The common “Western” diet — high in fried foods, refined grains, added sugars, and red meat — is associated with lower sperm counts and concentration and reduced sperm motility and normal morphology. In general, diets high in processed meats, such as hot dogs and cold cuts, are associated with lower sperm morphology. The consumption of trans fats, found in partially hydrogenated vegetable oils like margarine as well as in animal products, has also been associated with lower sperm concentrations. Diets high in added sugars are also associated with lower progressive sperm motility.
On the other hand, a diet high in fish, lean poultry, fruits and vegetables, legumes, and whole grains has been shown by multiple studies to be associated with improved sperm health, including better sperm motility. The “Mediterranean diet,” modeled on what’s traditionally eaten in Italy and Greece (primarily fruits and vegetables, seafood, healthy fats, and whole grains) is one example of a diet that has the potential to lead to sperm quality improvement, according to several studies.
We know that fruits and vegetables are key for sperm health and sperm quality, as they’re an excellent source of many of the vitamins, antioxidants, and nutrients required for the body to create healthy sperm, such as folic acid, vitamin C, vitamin E, and other antioxidants. Men who eat higher amounts of fruits and vegetables, particularly leafy greens, have a better chance of having higher sperm concentrations and improved motility.
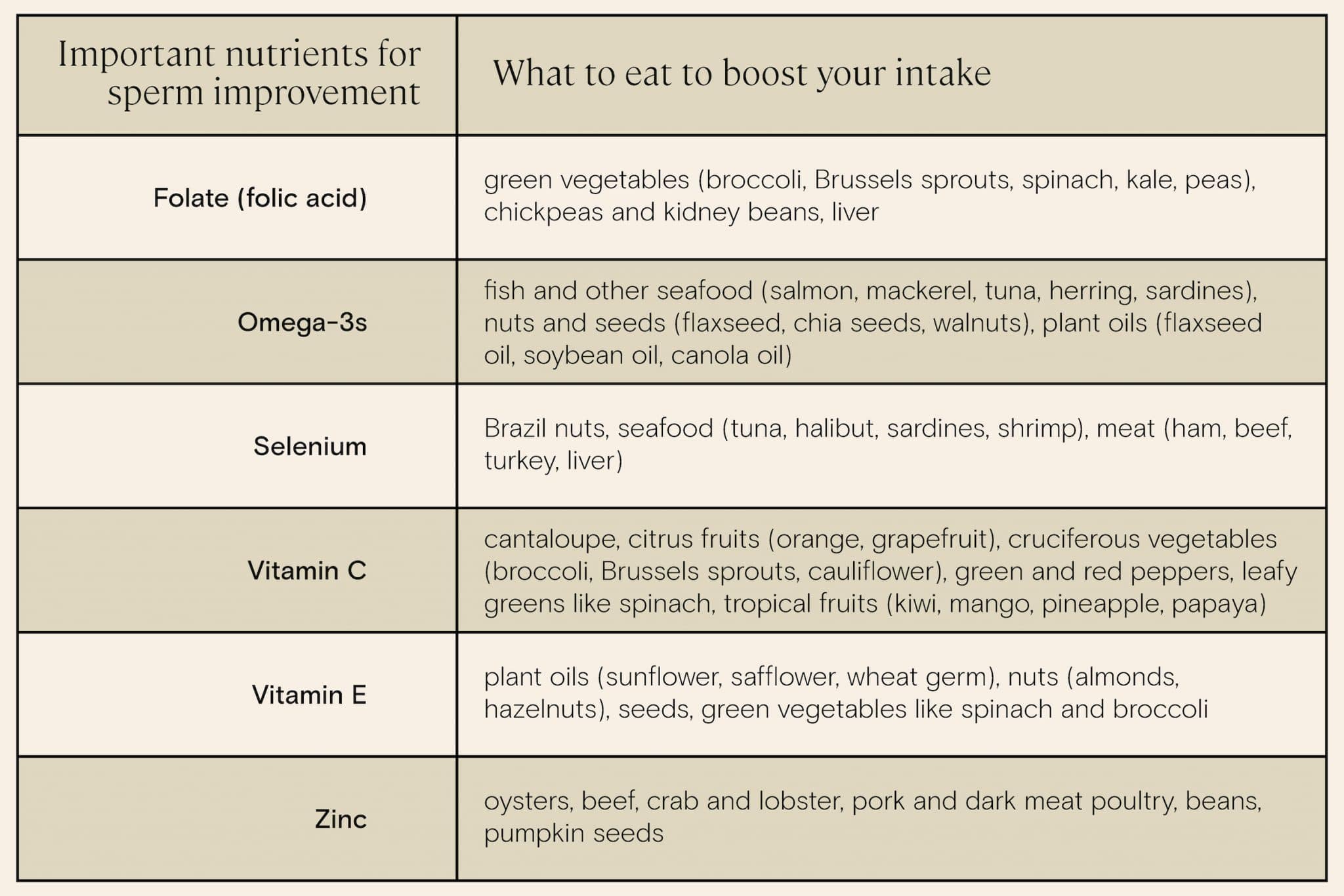
It’s best to get all the nutrients you need from your diet, but male fertility supplements and regular multivitamins can help fill in any gaps. Learn more about male fertility supplements.
We also know that the consumption of nuts, specifically walnuts, is associated with improved sperm parameters, including higher concentration, sperm motility improvement, sperm morphology improvement, and lower DNA fragmentation. Researchers believe this may be due to the nuts’ high levels of omega-3 and omega-6 fatty acids, which are important for sperm quality. Additionally, Brazil nuts are a great source of selenium, a trace mineral that plays a key role in reproductive health.
What about soy? Much has been made of the impact of this legume, a staple in many vegetarian and vegan diets. Soy products such as tofu, miso, and flavor compounds contain high levels of phytoestrogens, compounds that mimic the effect of estrogen in the body. One study found that a high intake — more than 2 servings per week — of soy foods was associated with lower sperm concentration, but not lower motility or morphology.
However, another study of IVF patients demonstrated that the male partner’s soy intake had no impact on fertilization rate, embryo quality, pregnancy rate, or live birth rate. While the research is inconclusive, it’s probably best to moderate your consumption of soy foods while trying to conceive.
Changing your diet for sperm improvement
The best potential sperm improvement diet is high in:
- Fruits and vegetables, specifically leafy greens and cruciferous vegetables like broccoli and Brussels sprouts
- Nuts and seeds such as walnuts, Brazil nuts, and pumpkin seeds
- Fatty fish such as salmon
And low in:
- Soy products
- Processed meats
- Red meat
- Added sugars
- Trans fats
Exercise and sperm health
Approximately a quarter of Americans live a sedentary lifestyle, meaning they don’t regularly engage in physical activity and have jobs that involve lots of sitting. We know that a sedentary lifestyle is associated with a negative impact on fertility (in addition to many other elements of overall health), and that regular exercise is associated with sperm quality improvement.
In one study of sperm donors, those who spent more time engaging in physical activity had increased progressive motility. In another, sperm motility improvement and sperm morphology improvement was noticed in physically active men. Active men also had healthier hormone profiles for fertility (including higher levels of testosterone, one of the hormones which drives the male reproductive system) when compared to their more sedentary counterparts.
Obesity and sperm health
Some of the sperm improvements found with exercise may come from shedding excess weight. Being overweight or obese has been associated in research with lower sperm count and decreased motility.
A 2016 study assessed male partners in subfertile couples, classifying them into four categories: underweight, normal, overweight, and obese. Researchers concluded that sperm quality, concentration, count, and motility were all slightly lower in overweight and obese participants than in those with normal weight. Additionally, rates of oligospermia (low sperm count) and azoospermia (sperm count of zero) were more prevalent among obese patients, compared with normal weight men.
Exercising for sperm improvement
Embarking on a regular exercise routine may have a remarkable effect on sperm improvement and sperm quality improvement. One study demonstrated that a 16-week aerobic training program, consisting of hour-long workouts on a treadmill three times a week, lead to improvement in the sperm count, motility and normal morphology of obese patients. It’s been shown in some studies that exercise can lead to significant sperm improvement in as little as a few months.
What type of exercise is best for sperm quality improvement? In one study, men who practiced physical activities such running or swimming at least 3 times per week had better sperm motility and morphology, and lower levels of dead or dying sperm in their semen samples.
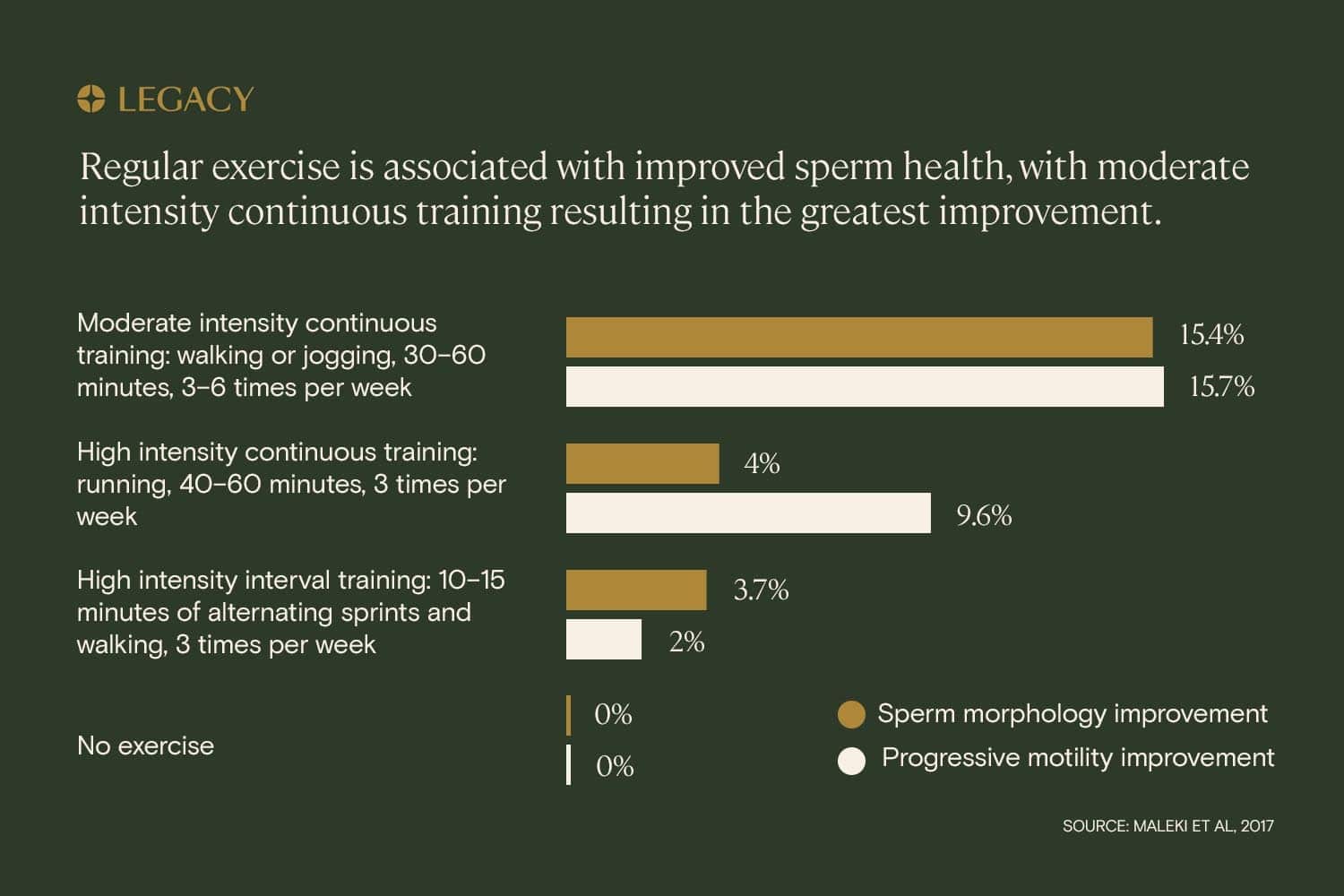
Another study measured the sperm improvement impact of several exercise regimens:
- Moderate intensity continuous training (30–60 minutes of walking or jogging, 4–6 times per week)
- High intensity continuous training (40–50 minutes of running, 3 times per week)
- High intensity interval training (alternating sprinting and recovery for 20–40 minutes, 3 times per week)
The study found that, while all of the above exercise regimens had positive effects on sperm health and sperm quality, the best exercise method for sperm improvement was moderate intensity continuous training. This suggests that sperm improvement can be seen by adopting the simple habit of walking or jogging most days of the week.
Exercise to avoid for sperm improvement
Interestingly, there are a few types of exercise that may negatively affect sperm health and sperm quality — and it’s possible for exercise to be too intense. Cycling, specifically, is what researchers call a “troublesome” activity for male fertility, due to the pressure on the testicles and its nerves and vessels from the bike seat, and the risk of the testicles being overheated. Cycling for five or more hours per week has been associated with reductions in sperm concentration and motility, and in one study, men who reported cycling for 1.5 hours or more per week had sperm concentrations that were 34% lower than those of men who did not ride bicycles.
Other high-intensity activities correlated with detrimental effects on sperm health include long-distance running such as marathons, vigorous training, and high-altitude mountain trekking.
Overall, a moderate approach to physical activity is recommended for sperm improvement and male fertility improvement.
Learn more about exercise and sperm health and how activity can lead to sperm quality improvement.
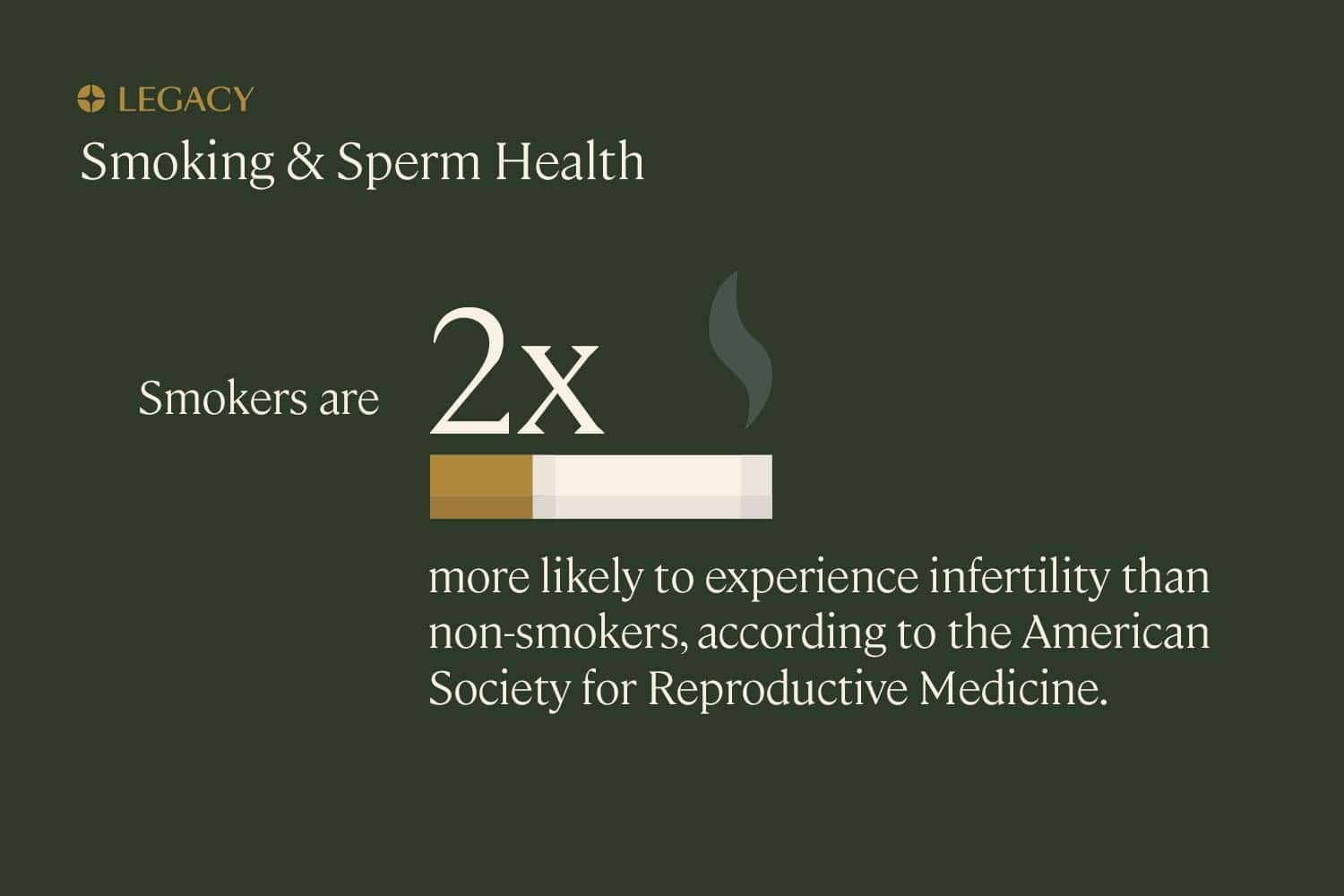
Smoking and sperm health
Cigarette smoking has long been considered one of the leading risk factors in male-factor infertility. A 2016 review examined 20 different studies of tobacco use and its effects on sperm health, and found that smoking was associated with significantly reduced sperm count and motility — and that the more you smoke, the stronger these effects are. This was reinforced by a 2019 review that found a strong correlation between smoking and low sperm count/poor morphology.
According to the American Society for Reproductive Medicine (ASRM), infertility rates among smokers (both male and female) are twice as high as among non-smokers. Additionally, because smoking has the potential to damage the genetic health of sperm, those who smoke have a higher risk of having difficulty conceiving naturally, parenting a pregnancy that ends in miscarriage, or going through an unsuccessful IUI or IVF cycle.
If you quit smoking, there’s evidence that it can lead to sperm improvement. In one follow-up study of men who quit smoking, sperm motility improvement and morphology improvement was noted within an average of six months. Research shows that former smokers who quit more than six months ago have similar semen parameters to non-smokers.
Learn more about smoking and sperm health and how tobacco can impact sperm quality.
Alcohol and sperm health
The relationship between alcohol consumption and sperm quality is a bit complex. We do know that high alcohol consumption is associated with decreased sperm health and sperm quality, with negative impacts on all sperm parameters. Habitual binge drinking is especially detrimental to sperm health — in one study, men who drank more than 40 drinks per week had a 33% reduction in sperm concentration compared to men who drank fewer than 5 drinks per week.
However, it may not be necessary to completely remove alcohol from your life in order to improve your sperm quality. It’s actually possible, according to some research, that some alcohol consumption may actually have fertility benefits (experts hypothesize that’s because some alcohol, like wine and whiskey, contains antioxidants).
Additionally, it appears that occasional and social drinking has no significant impact on sperm health and sperm quality. If you’re looking for sperm improvement, you should consider limiting alcohol consumption to fewer than 5 drinks per week.
Learn more about drinking and sperm health and how alcohol can impact sperm quality.
Drugs, medications, and sperm health
Certain drugs and medications — whether prescription or not — are associated with reduced sperm quality and sperm count.
Medications that may impact male fertility include, but are not limited to:
- Chemotherapy drugs
- SSRIs and similar antidepressants
- Alpha blockers
- Ketoconazole
- Some antibiotics
- 5-alpha-reductase inhibitors
- Opiates
- NSAIDs
- Corticosteroids
- Antipsychotics
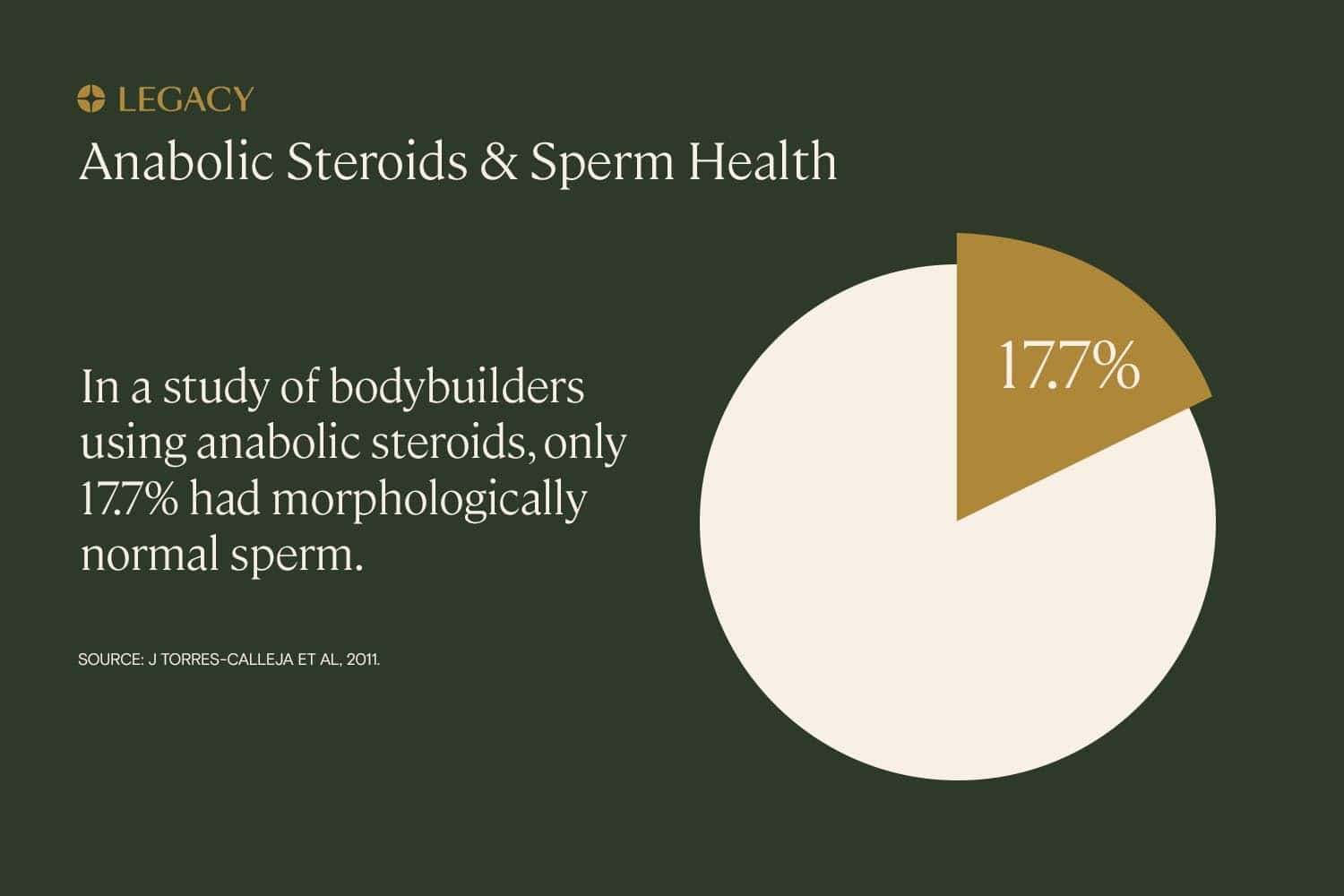
Anabolic steroids and sperm health
Anabolic steroids, also known as “performance-enhancing” drugs, are typically natural or synthetic forms of testosterone, often used to rapidly increase muscle mass. It might seem that — since testosterone is the hormone that controls the male reproductive system — adding testosterone to the body would improve fertility.
In fact, the opposite is true. Injecting additional testosterone actually causes the body to believe there’s enough testosterone. This signals the testes to stop the internal production of testosterone, which has long-term detrimental effects on spermatogenesis and sperm quality.
Long-term use of steroids is associated with drastically lower percentages of motile and morphologically normal sperm, reaching zero sperm count in many instances. For many steroid users, sperm improvement can be seen within 4–12 months of stopping the drugs; this recovery process can be assisted with certain medications.
However, a subgroup of men might have irreversible damage to their sperm production despite all medical interventions. Some users experience steroid-induced “hypogonadism,” or a shutdown of the function of the testes, which produce testosterone and are responsible for creating sperm.
Avoiding – or stopping – steroids can lead to male fertility improvement as well as sperm quality improvement.
Sperm improvement medications
If you have low sperm count or poor motility/morphology and you’ve attempted sperm improvement on your own without any change, it may be time to see a specialist. Fertility specialist urologists and andrologists are the best qualified to treat male fertility issues, and can help diagnose male-factor infertility problems and treat them medically.
Depending on the etiology of male infertility, some fertility medications may be effective for male fertility improvement and sperm quality improvement. These aren’t solutions you can undertake on your own. These medications are prescribed by a doctor for specific, diagnosed causes of reduced fertility.
Three of the most common medications for sperm improvement and sperm quality improvement:
- Clomiphene citrate (or “Clomid”) is an estrogen receptor modulator medication that, when used to treat male infertility, can increase levels of internal testosterone and promotes spermatogenesis—all of which contribute to the production of sperm. Clomid has been shown to improve sperm count/concentration and motility in some men experiencing reduced fertility.
- Anastrozole is a medication that has a similar effect, decreasing estrogen levels and increasing levels of testosterone to support sperm production. This medication may help improve sperm health for those who have low sperm count, and has been shown to improve sperm motility as well.
- Finally, human chorionic-gonadotropin (hCG) and human menopausal gonadotropin (hMG) are two injectable hormone medications also used to treat hormone imbalances in testosterone and LH that lead to low sperm count and other fertility issues.
Learn more about treatments for male fertility.
References
- Practice Committee of the American Society for Reproductive Medicine. “Diagnostic evaluation of the infertile male: a committee opinion.” Fertility & Sterility, 2015.
- Hagai Levine et al. “Temporal trends in sperm count: a systematic review and meta-regression analysis.” Human Reproduction Update, 2017.
- Aura María Gil-Villa et al. “Assessment of sperm factors possibly involved in early recurrent pregnancy loss.” Fertility & Sterility, 2010.
- Feiby L. Nassan, ScD, MBBCh, MSc et al. “Association of Dietary Patterns With Testicular Function in Young Danish Men.” Urology, 2020.
- M. Afeiche et al. “Meat intake and semen parameters among men attending a fertility clinic.” Fertility & Sterility, 2013.
- Jorge E. Chavarro, MD, ScD et al. “Trans fatty acid levels in sperm are associated with sperm concentration among men from an infertility clinic.” Fertility & Sterility, 2012.
- Y. H. Chiu et al. “Sugar-sweetened beverage intake in relation to semen quality and reproductive hormone levels in young men.” Human Reproduction, 2014.
- Albert Salas-Huetos et al. “Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies.” Human Reproduction Update, 2017.
- Audrey J. Gaskins et al. “Dietary patterns and semen quality in young men.” Human Reproduction, 2012.
- Dimitrios Karayiannis et al. “Association between adherence to the Mediterranean diet and semen quality parameters in male partners of couples attempting fertility.” Human Reproduction, 2017.
- A Cutillas-Tolín et al. “Mediterranean and western dietary patterns are related to markers of testicular function among healthy men.” Human Reproduction, 2015.
- Daniela Paes de Almeida Ferreira Braga et al. “Food intake and social habits in male patients and its relationship to intracytoplasmic sperm injection outcomes.” Fertility & Sterility, 2012.
- Albert Salas-Huetos et al. “Effect of nut consumption on semen quality and functionality in healthy men consuming a Western-style diet: a randomized controlled trial.” The American Journal of Clinical Nutrition, 2018.
- Wendie A. Robbins et al. “Walnuts improve semen quality in men consuming a Western-style diet: randomized control dietary intervention trial.” Biology of Reproduction, 2012.
- Jorge E. Chavarro et al. “Soy food and isoflavone intake in relation to semen quality parameters among men from an infertility clinic.” Human Reproduction, 2008.
- Lidia Mínguez-Alarcón et al. “Male soy food intake was not associated with in vitro fertilization outcomes among their partners attending a fertility center.” Andrology, 2016.
- Bin Sun et al. “Physical activity and sedentary time in relation to semen quality in healthy men screened as potential sperm donors.” Human Reproduction, 2019.
- Diana Vaamonde et al. “Physically active men show better semen parameters and hormone values than sedentary men.” European Journal of Applied Physiology, 2012.
- Miguel Ángel Rosety et al. “Exercise improved semen quality and reproductive hormone levels in sedentary obese adults.” Nutrición Hospitalaria, 2017.
- Paula C. Lalinde-Acevedo et al. “Physically Active Men Show Better Semen Parameters than Their Sedentary Counterparts.” International Journal of Fertility and Sterility, 2017.
- Behzad Hajizadeh Maleki et al. “The effects of three different exercise modalities on markers of male reproduction in healthy subjects: a randomized controlled trial.” Reproduction, 2017.
- Paweł Jóźków, MD et al. “The Impact of Intense Exercise on Semen Quality.” American Journal of Men’s Health, 2017.
- Reecha Sharma et al. “Cigarette Smoking and Semen Quality: A New Meta-analysis Examining the Effect of the 2010 World Health Organization Laboratory Methods for the Examination of Human Semen.” European Urology, 2016.
- Pravesh Kumar Bundhun et al. “Tobacco smoking and semen quality in infertile males: a systematic review and meta-analysis.” BMC Public Health, 2019.
- Harald Trummer et al. “The impact of cigarette smoking on human semen parameters and hormones.” Human Reproduction, 2002.
- C H Ramlau-Hansen et al. Is smoking a risk factor for decreased semen quality? A cross-sectional analysis.” Human Reproduction, 2007.
- Tina Kold Jensen et al. “Habitual alcohol consumption associated with reduced semen quality and changes in reproductive hormones; a cross-sectional study among 1221 young Danish men.” BMJ Open, 2014.
- E. Ricci et al. “Alcohol intake and semen variables: cross‐sectional analysis of a prospective cohort study of men referring to an Italian Fertility Clinic.” Andrology, 2018.
- Daniela Marinelli et al. “Mini-review of studies on the effect of smoking and drinking habits on semen parameters.” International Journal of Hygiene and Environmental Health, 2004.
- Elena Ricci et al. “Semen quality and alcohol intake: a systematic review and meta-analysis.” Reproductive BioMedicine Online, 2017.
- U. A. Knuth et al. “Anabolic steroids and semen parameters in bodybuilders.” Fertility & Sterility, 1989.
- J Torres-Calleja et al. “Effect of androgenic anabolic steroids on sperm quality and serum hormone levels in adult male bodybuilders.” Life Science, 2001.
- Simantini S Patankar et al. “Effect of clomiphene citrate on sperm density in male partners of infertile couples.” Indian Journal of Physiology and Pharmacology, 2007.
- Jay D. Raman et al. “Aromatase inhibitors for male infertility.” Journal of Urology, 2002.
- Ali A. Dabaja et al. “Medical treatment of male infertility.” Translation Andrology and Urology, 2014.