Men’s Guide to Trying to Conceive
If you feel like the only thing you ever learned about pregnancy was how to prevent it, you’re not alone. Many cis men don’t know much about the process of trying to conceive other than that it involves sex — but when? How much? And what can be done to increase the odds of achieving pregnancy?
Our Men’s Guide to Trying to Conceive will give you everything that you need to know about the male side of conception, step by step.
The guide below is specifically for cisgender men in heterosexual relationships. However, families come in many forms and Legacy supports them all. Learn more about LGBTQ fertility options.

Planning for pregnancy
We often think about the female partner as being the only one who needs to physically “prepare” for pregnancy. However, sperm is half of the equation — and sperm health can affect fertility, chances of miscarriage, and even the health of your offspring. Here are some steps to understanding and improving the health of your sperm, your overall fertility, and the male side of conception.
Check in on your fertility health
A 2021 survey revealed that 73% of men who are trying to conceive or thinking about starting a family have no knowledge of their sperm quality.
People with a menstrual cycle get a monthly message from their bodies that can alert them to any fertility “red flags.” Irregular, very light, or heavy menstrual cycles can all be signs of hormone imbalance, ovulation disorders, or endometriosis, all of which can affect a person’s chances of conceiving.
Male infertility symptoms are not so obvious. There are a handful of possible male infertility symptoms, but for the most part, you may not know there’s an issue with your sperm health until you’re trying to conceive or being evaluated for infertility by a specialist.
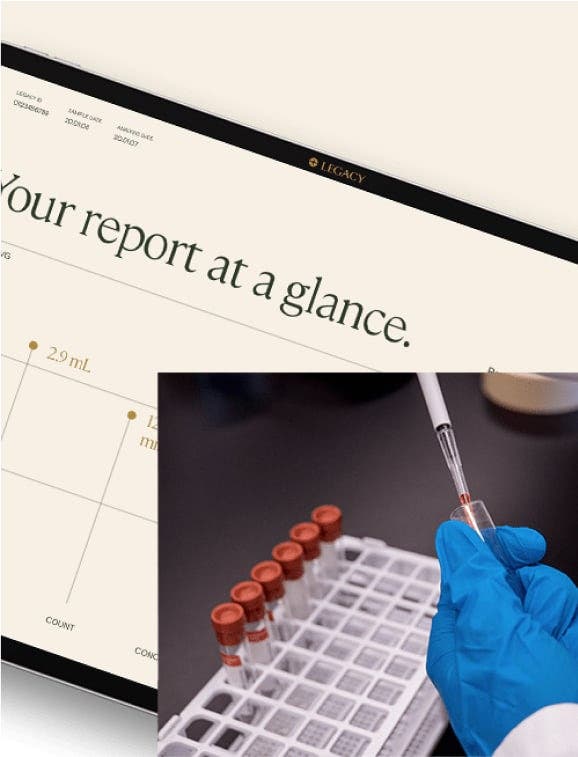
That’s why we recommend proactive male fertility testing. Semen analysis is the cornerstone of male fertility testing; this simple lab analysis can determine your sperm count (how many sperm you have), motility (how many of those sperm are moving), and morphology (how many of those sperm are the proper shape).
All too often, men’s fertility isn’t tested at all until a couple has been trying for 12 months. Male fertility issues contribute to half of infertility cases — and in many instances, can be addressed with simple lifestyle changes. Testing early in the process of trying to conceive can help you avoid costly and unnecessary tests or treatments down the line. Additionally, it can help you choose lifestyle interventions or treatments that address your specific needs and quickly diagnose male infertility symptoms.
Other preconception testing
In addition to a semen analysis, the following tests may be appropriate for you, depending on your personal health history.
Genetic testing
For those who have a family history or a predisposition for certain genetic disorders (such as cystic fibrosis, Tay-Sachs, or sickle cell anemia), genetic testing known as “carrier screening” may be appropriate before trying to conceive.
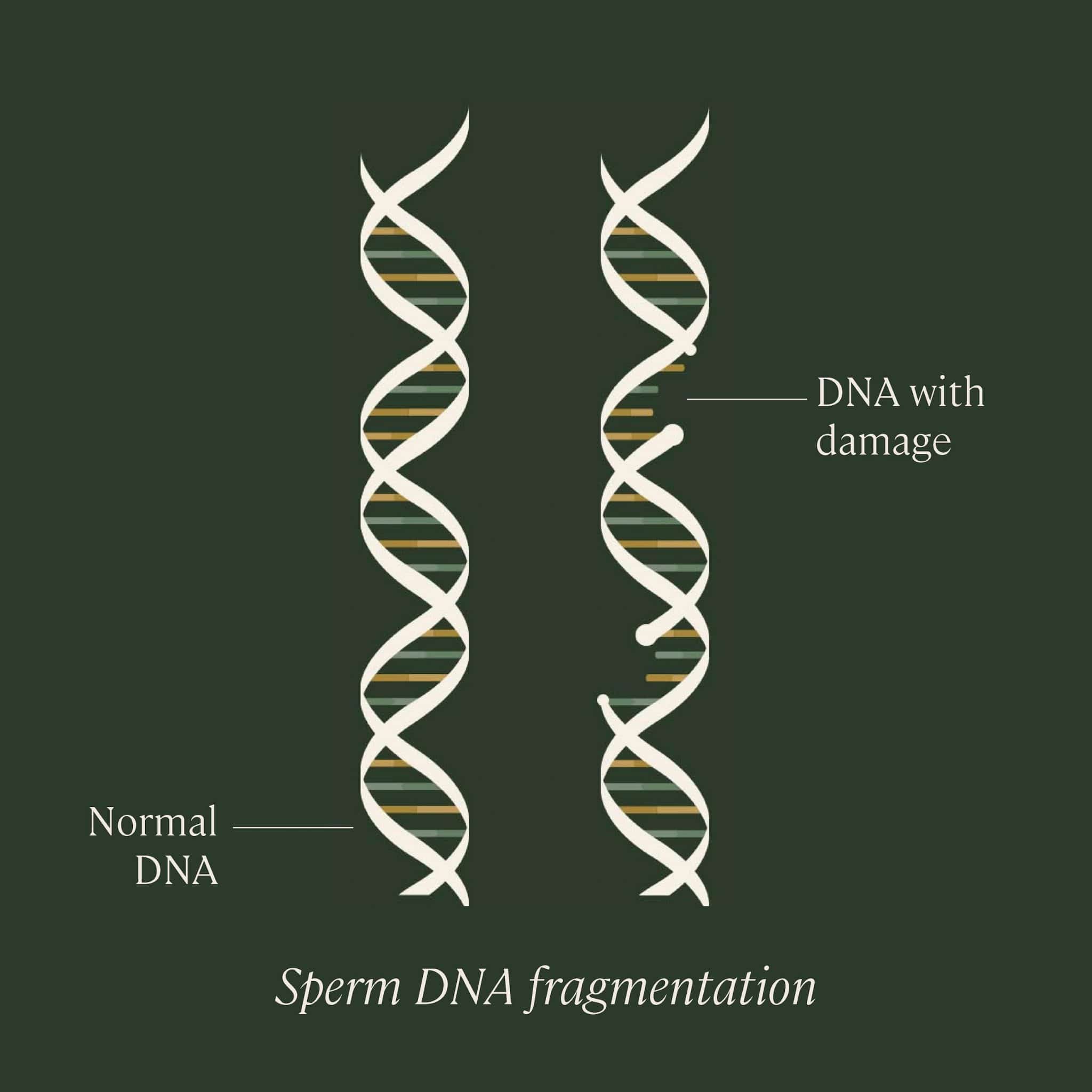
Sperm DNA fragmentation testing
Sperm DNA fragmentation refers to the degree of damage to the genetic material carried by sperm — the genetic material that will hopefully become half of your future child.
Damage to sperm DNA can occur for a number of reasons, such as smoking or illness, which cause oxidative stress in the body. Research shows that sperm with a high level of DNA fragmentation is correlated with lower pregnancy rates and higher miscarriage rates.
A sperm DNA fragmentation analysis will provide you with a DNA fragmentation index (DFI), which is the percentage of your sperm with damaged DNA. There are a few risk factors that may increase the likelihood of a high DFI, such as:
- Advanced paternal age (if you’re over the age of 40)
- Smoking
- History of illness or infections (cancer, influenza, STIs)
- Chemical, toxin, or radiation exposure
If you have any of the risk factors outlined above, if you’ve been trying to conceive for 6–12 months, are starting fertility treatments, or have experienced multiple miscarriages, then it may be a good idea for you to get a sperm DNA fragmentation analysis.
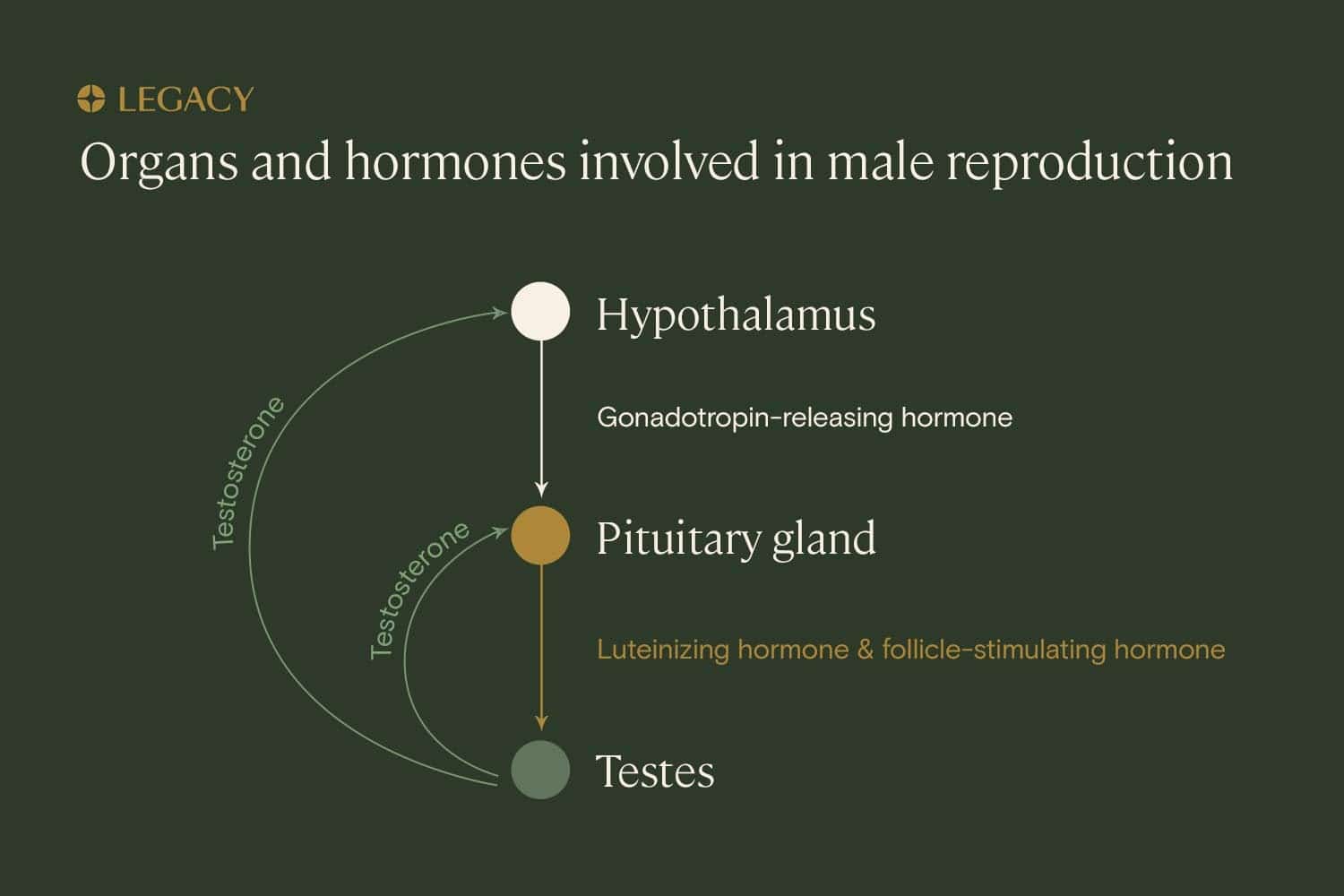
Male fertility hormone testing
Hormone production plays an important role in fertility. Testosterone is the hormone most people associate with male fertility and male conception, but there are two other very important hormones that work together with testosterone to help produce sperm: follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
Abnormal levels of any of these hormones may have an impact on male fertility. For example, low levels of FSH may cause a patient to produce low numbers of sperm (or no sperm at all). LH is responsible for releasing testosterone, so if there is an imbalance there, your body may not be releasing the testosterone necessary to help sperm develop.
If you have received results from a sperm analysis that show low sperm count or poor sperm health — or if you’ve been experiencing a decrease in libido or issues with sexual function — hormone imbalance could be the culprit, and hormone testing may be appropriate.
Improving your fertility before trying to conceive
Your body is producing sperm constantly from the time you hit puberty. As a result, your recent lifestyle can have a big impact on your sperm health. If you are trying to conceive or want to improve your fertility, here are some lifestyle factors you should consider.
Remember: it takes about 74 days to produce sperm. So if you implement any lifestyle changes, it may be 2–3 months before you see those improvements reflected in your sperm health or semen analysis results.
Learn more in our Guide to Sperm Improvement.

Diet to
improve male fertility
A diet rich in fruits and vegetables, whole grains, and healthy fats (such as what’s found in seafood and nuts) — and low in refined grains, processed meats, and added sugar — is associated with improved fertility. The meat-and-potatoes (and pizza and soda and fries) “Western diet” most of us are familiar with is likely detrimental to sperm, research shows.
If you’re looking for specific foods to increase male fertility, know it’s not that simple; it’s much more about patterns than about consuming one individual ingredient. But a good template can be found in the Mediterranean diet, based on the eating habits of those living in Greece, Italy and Spain. This diet, composed primarily of fruits and vegetables, seafood, healthy fats, and whole grains, has been shown to improve sperm health and pregnancy rates.

Male
conception supplements
Vitamins and supplements can help fill in the gaps in our diets. There are several male conception supplements that can benefit male fertility by boosting sperm count, improving motility or morphology, or increasing testosterone levels.
One example of a male conception vitamin is CoQ10 and other antioxidants, which appear to help protect sperm from the oxidative stress caused by pollution, illness, poor diets, and more. Another is folate, a nutrient that’s critical to cell division and development and is associated with improved semen parameters.
Learn more about male fertility supplements.

Exercise to
improve male fertility
Regular physical activity is associated with improved semen parameters, as well as healthier hormone profiles for fertility (such as higher levels of testosterone). But you don’t have to become a marathon runner overnight to enhance your sperm health.
The best exercise for sperm health is actually the most straightforward: the simple habit of walking or jogging for at least 30 minutes, 3–6 times per week has been shown to have the greatest benefit for sperm motility and morphology.

Evaluate smoking and drinking habits
We know that smoking and drinking is a no-no for women who are trying to get pregnant. But what about their partners?
Cigarette smoking has long been considered one of the leading factors in male-factor infertility. Extensive research has determined that smoking is associated with significantly reduced sperm count and quality. If you quit smoking, your fertility may improve fairly quickly, beginning to return to normal within six months. If you’re planning to or trying to conceive right now, you should quit smoking as soon as possible.
When it comes to alcohol, you don’t need to quit altogether. Research tells us that occasional, moderate drinking has no serious effect on fertility. But habitual binge drinking is detrimental to sperm health, so keeping it under 5 drinks per week is best.

Evaluate
your medication usage
Some medications have the unintended side effect of affecting testosterone levels or spermatogenesis, the process of sperm production in the testicles. While this isn’t an issue on a day-to-day basis, it may become one if you and your partner are trying to conceive. Antidepressants, antipsychotics, alpha blockers, antifungals, antibiotics, hair loss medications, Viagra, opiates, and steroids have all been associated with reduced sperm count and sperm quality.
Trying to conceive
Contrary to what you were likely taught in high school sex ed, you can’t just get your partner pregnant any day of the month. Conception is slightly more complex than it seems.
In order to conceive a healthy pregnancy, a couple needs three things:
- A healthy egg to be ovulated
- A healthy sperm to make it to, and fertilize, the egg at the right time
- A healthy uterus to accept the fertilized egg
Identifying the “fertile window” and ovulation
The fertile window is the period during which a person can get pregnant. This window is the day an egg is released from the ovaries (ovulation) and the five days beforehand. This time period offers couples looking to conceive the best chance of getting pregnant naturally.
Overview of the average monthly menstrual and ovulation cycle
- Day 1–4: Menstruation. This is the period in which the uterine lining from the month before is shed to prepare for a new cycle.
- Day 1–14: Follicular phase. During this phase, hormones prompt the development of the ovarian follicles, which contain eggs. Typically, only one egg will become mature and ready to be ovulated.
- Day 10–15: The fertile window. This is the period in which unprotected sex is most likely to result in pregnancy. Sperm can live in the female reproductive system for up to five days, so the five days leading up to ovulation and the one day after should all be considered “fertile” days. However, the 2–3 days before ovulation are optimal for intercourse if you’re trying to conceive.
- Day 14: Ovulation. This is the process by which the mature egg is released from the ovary. Then, it travels down the fallopian tube, where it may meet with sperm and become fertilized. If the egg does not become fertilized within 12–24 hours of ovulation, it will disintegrate.
- Day 15–29: The luteal phase. During this phase, hormones prompt the uterine lining to thicken. If the egg is fertilized, it can implant in the uterine lining about a week later. That’s when hCG, the “pregnancy hormone,” will begin to be produced. If the egg is not fertilized, toward the end of the luteal phase, the body will prepare to shed the lining and start again.
Note: This timeline is based on a 28–29 day cycle, which is average. Your partner may have cycles between 21 and 35 days long, and phases will adjust accordingly. The luteal phase is typically around 12–14 days long, but the follicular phase can be as short as 7 or as long as 21.
How to identify the fertile window
There are few methods you and/or your partner can use to identify the fertile window and determine the best time to have sex if you’re trying to conceive.
- Cycle tracking. If your partner uses an app or a calendar to track her menstrual cycle, that can give her a rough idea of when she may ovulate. Not every cycle is 28 days long, and ovulation doesn’t always occur exactly halfway through the menstrual cycle.
Keep in mind that the luteal phase, the final phase before the period, typically stays about 12–14 days long and directly follows ovulation. So, if she usually has a 32-day cycle, she is likely to be ovulating around day 18; in a 24-day cycle, it will be around day 10.
- Basal body temperature monitoring. Basal body temperature (BBT) is the body’s resting temperature. When a woman is ovulating, her BBT will rise slightly — about half a degree — and remain higher until her next period. Some women also experience a little dip in BBT just before ovulation, though this is not universal. By charting BBT over several months, your partner can identify which day she’s ovulating and count back to determine her fertile window.
She can check her BBT by taking her temperature with a thermometer every morning before she gets out of bed. Or, she can use a wearable like the Ava tracker to automatically record BBT and alert her to her fertile window.
- Ovulation prediction kits. Ovulation prediction kits or “OPKs” use urine test strips that identify luteinizing hormone. In women, this hormone surges about 24–36 hours before ovulation. When your partner gets a positive ovulation test, you should plan to have sex that day.
It’s helpful to test frequently so you don’t miss the ovulation window; many women start testing on day 8, if they have shorter or irregular cycles, or day 10–11 if they have average or longer cycles.
Remember: The best time to have sex when you’re trying to conceive is within the three days prior to ovulation. So while these methods can pinpoint your partner’s ovulation date within a particular cycle, it’s helpful to look at a few month’s worth of data and use that to determine her most likely fertile window.
How often should we have sex?
If you are trying to conceive, you and your partner should be having sex at least every other day during the fertile window.
- If you have normal sperm count and quality, every other day during the fertile window is fine.
- If you have low sperm count or poor sperm quality, every day or even multiple times per day during the fertile window.
Let’s explain:
A 1995 research article from the New England Journal of Medicine suggested that for couples without fertility challenges, sex every day during the fertile window gave them a 25% chance of conceiving. Sex every other day? 22%. So, men with normal sperm counts can have sex every other day during the fertile window and still have a good chance of impregnating their partner.
But for men with low sperm counts or sperm quality issues, the advice changes.
Men with low sperm counts have a better chance of conceiving by having sex every day during their partner’s fertile window. This might be contrary to common sense, since it seems like men with low sperm count should “save up” their sperm, but several studies have suggested that shorter abstinence windows specifically benefit men with low sperm count.
One study of over 9,400 semen samples from over 6,000 patients suggest that, for men with low sperm count, peak sperm motility was reached after just one day of abstinence.
Interestingly, having intercourse multiple times per day might help even more. A study of 576 men at an infertility and IVF unit examined the semen analysis results of men ejaculating twice in a 1–4 hour period. This study found that, in contrast to men with normal fertility, men with low sperm counts had no significant difference in the number of sperm produced in the second sample. The “pooled” samples significantly increased the total sperm count, potentially increasing the chance of pregnancy.
Another small study in 2016 had similar results, concluding that, for men with low sperm count, ejaculating twice in one hour produced more normal sperm and better motility in the second ejaculation.
How conception works
Let’s say your partner has ovulated, and you’ve had sex within her fertile window — what happens next?
Let’s say your partner has ovulated, and you’ve had sex within her fertile window — what happens next?
Fertilization is a “race to the top” of the female reproductive system, from the vagina to the fallopian tubes, where sperm meet the egg and fertilization occurs. On average, anywhere between 80 and 300 million sperm cells are released per ejaculation. However, most are eliminated along the way.
The journey to the egg is full of obstacles. The acidic environment of the vagina will eliminate sperm that linger for too long. Once sperm reach the cervix, they must navigate through mucus that can trap many (though this mucus typically thins during a woman’s fertile window). Sperm can be lost to “crypts,” side-channels of the cervix where they can survive for several days.
Once they reach the fallopian tubes, many become bound to its surface. Only a select few continue on to the egg — that is, if they’ve chosen the correct tube.
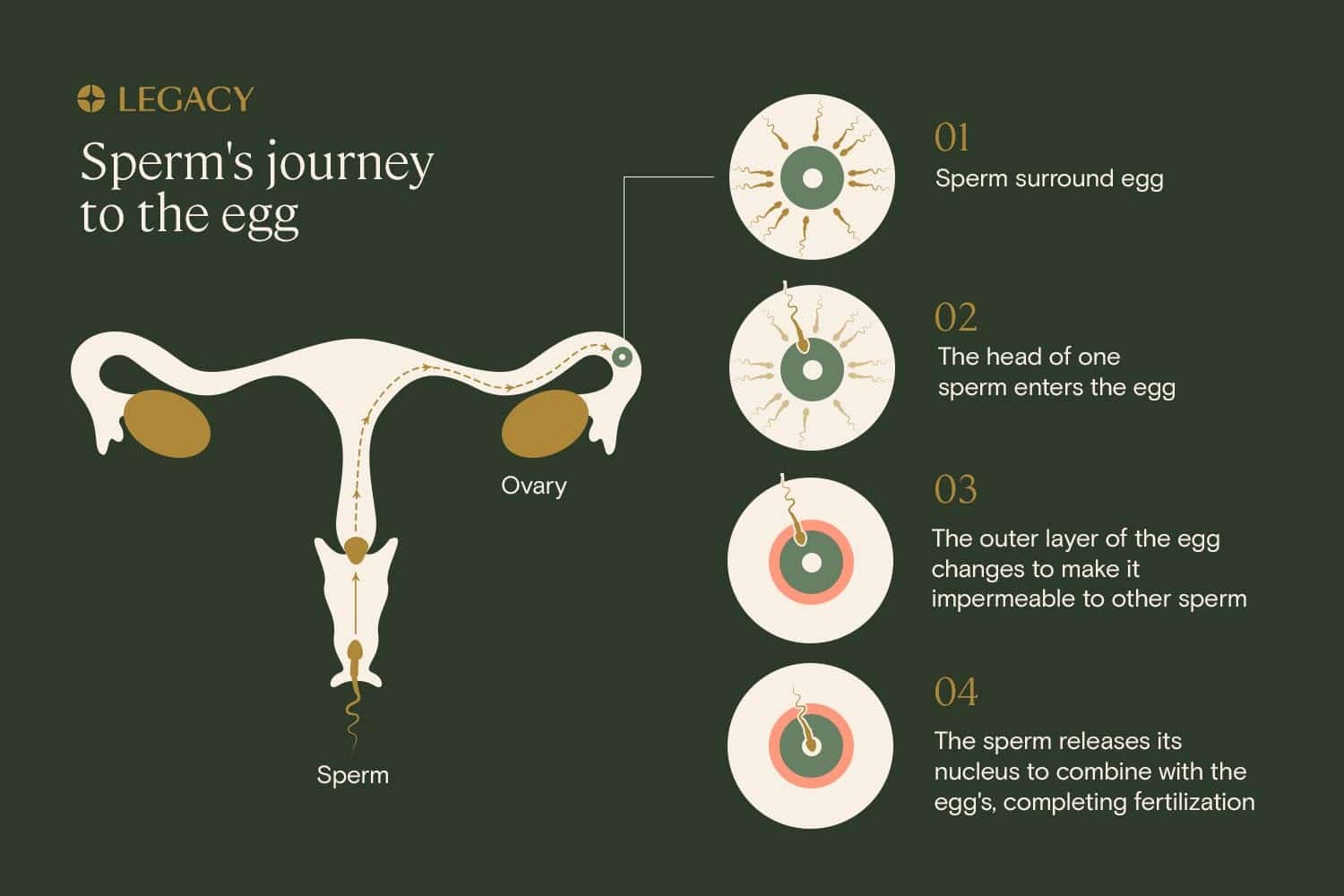
Abnormal or otherwise defective sperm fall to the many dangers of the journey, along with a good percentage of healthy sperm. In fact, less than 1 in a million from the original ejaculate will reach the egg at the time of fertilization. It is hypothesized that this long, arduous journey is nature’s way of weeding out the weak, so only the healthiest, strongest sperm survive.
When a sperm reaches the upper part of the female reproductive system, it undergoes the final steps that allow it to fertilize the egg: chemical changes to the surface of the sperm allow it to dissolve the egg’s outer layer, and the sperm tail begins to “beat” faster to facilitate egg penetration. After the sperm penetrates to the cytoplasm of the egg cell, it releases its nucleus to combine with the egg’s. Immediately, the external layer of the egg, known as the zona pellucida, changes to become impermeable to additional sperm.
After fertilization, the zygote — the term for a fertilized egg — will travel down the fallopian tubes and into the uterus. It can implant in the uterus approximately a week after fertilization. It’s at this point that the body starts producing human chorionic gonadotropin or hCG, the “pregnancy hormone.” Typically, hCG levels become high enough to get a positive result on an at-home pregnancy test around 10–14 days after ovulation, or around the day of her missed period.
How long should it take to get my partner pregnant?
How long it takes to get pregnant will depend on a number of factors, including your age, her age, and both of your personal fertility health. However, there are some basic statistics we can look to for guidance:
According to research:
- 30% of couples who are trying to conceive get pregnant within the first cycle (about one month).
- 60% get pregnant within 3 cycles.
- 80% get pregnant within 6 cycles.
- 85% get pregnant within 12 cycles (about one year).
If your female partner is over 35, it may take longer to get pregnant (think a year or more). That’s because a higher proportion of her eggs are genetically abnormal and unable to result in a healthy pregnancy.
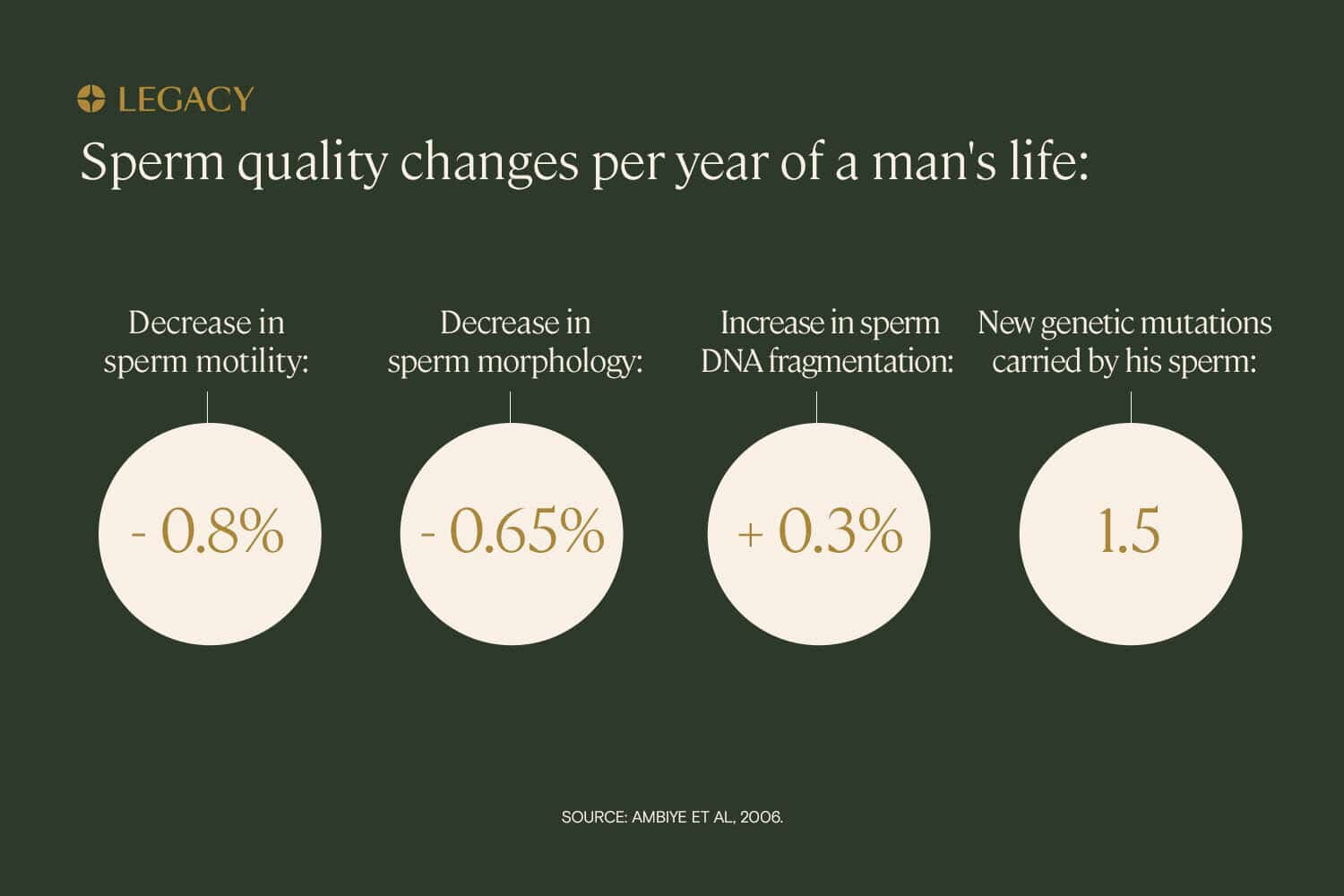
Men’s age affects time to conception as well. Research demonstrates that a couple with a male partner who is over 40 is 30% less likely to conceive within a year, compared to couples with a male partner who is 30 (regardless of the age of their female partner). That’s because sperm quality declines with age.
What to do if you’re not getting pregnant
If you have been actively trying to conceive — having sex frequently during your partner’s fertile window — and you’re not getting any positive pregnancy test results, you may be wondering: When should I seek help from a specialist?
When should we see a fertility specialist?
The traditional advice:
- If the female partner is under age 35, try for 12 months before seeking a fertility consultation.
- If the female partner is over age 35, try for 6 months before seeking a fertility consultation. That’s because women over 35 are more likely to experience infertility, and time is very valuable for them.
However, you might consider seeing a specialist earlier, if any of the following apply to you or your partner:
- If you’ve had multiple miscarriages.
- If you’ve had two or more abnormal semen analysis tests.
- If you or your partner has been diagnosed with a fertility-related issue, such as PCOS, endometriosis, varicocele, or congenital absence of the vas deferens.
- If you or your partner has a medical history that might affect fertility, such as a history of cancer or delayed puberty.
What type of fertility specialist should we see?
Typically, you’ll want to start by talking to your partner’s OB/GYN. While OB/GYNs are not fertility specialists, they can help diagnose some less complex fertility problems, prescribe some treatments, and refer to male fertility or female fertility specialists.
- Reproductive endocrinologist. A reproductive endocrinologist is a medical specialist in reproductive endocrinology and infertility (REI). A reproductive endocrinologist is an OB/GYN with advanced training in hormones, the science of fertility and the mechanics of conception, including sperm, eggs, male and female anatomy, and the relationship between pituitary and reproductive hormones. Reproductive endocrinologists can diagnose and treat infertility and perform fertility treatment such as IVF.
- Male fertility (andrologist) urologist. A urologist is a medical professional that diagnoses and treats conditions relating to the urinary tract in both males and females. For male fertility issues, it’s best to see an andrologist-urologist, a urologist who has a particular specialty in the male reproductive system, sperm health, and treating male infertility symptoms.
Couples dealing with male fertility issues will often see a urologist in tandem with a reproductive endocrinologist or OB/GYN.
References
- ExSeed Health. “ExSeed puts men’s fertility at the forefront with their at-home sperm tests.” Press release, 2021.
- Albert Salas-Huetos et al. “Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies.” Human Reproduction Update, 2017.
- Feiby L. Nassan, ScD, MBBCh, MSc et al. “Association of Dietary Patterns With Testicular Function in Young Danish Men.” Urology, 2020.
- Audrey J. Gaskins et al. “Dietary patterns and semen quality in young men.” Human Reproduction, 2012.
- A Cutillas-Tolín et al. “Mediterranean and western dietary patterns are related to markers of testicular function among healthy men.” Human Reproduction, 2015.
- Marijana Vujkovic et al. “The preconception Mediterranean dietary pattern in couples undergoing in vitro fertilization/intracytoplasmic sperm injection treatment increases the chance of pregnancy.” Fertility & Sterility, 2010.
- Sedigheh Ahmadi et al. “Antioxidant supplements and semen parameters: An evidence based review.” International Journal of Reproductive Biomedicine, 2016.
- Morvarid Irani et al. “The Effect of Folate and Folate Plus Zinc Supplementation on Endocrine Parameters and Sperm Characteristics in Sub-Fertile Men: A Systematic Review and Meta-Analysis.” The Journal of Urology, 2017.
- Diana Vaamonde et al. “Physically active men show better semen parameters and hormone values than sedentary men.” European Journal of Applied Physiology, 2012.
- Behzad Hajizadeh Maleki et al. “The effects of three different exercise modalities on markers of male reproduction in healthy subjects: a randomized controlled trial.” Reproduction, 2017.
- Pravesh Kumar Bundhun et al. “Tobacco smoking and semen quality in infertile males: a systematic review and meta-analysis.” BMC Public Health, 2019.
- Harald Trummer et al. “The impact of cigarette smoking on human semen parameters and hormones.” Human Reproduction, 2002.
- Elena Ricci et al. “Semen quality and alcohol intake: a systematic review and meta-analysis.” Reproductive BioMedicine Online, 2017.
- Tina Kold Jensen et al. “Habitual alcohol consumption associated with reduced semen quality and changes in reproductive hormones; a cross-sectional study among 1221 young Danish men.” BMJ Open, 2014.
- Jonathan R. Bull et al. “Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles.” npj Digital Medicine, 2019.
- Kaitlyn Steward et al. “Physiology, Ovulation And Basal Body Temperature.” StatPearls, updated 2021.
- Allen J. Wilcox, MD et al. “Timing of Sexual Intercourse in Relation to Ovulation — Effects on the Probability of Conception, Survival of the Pregnancy, and Sex of the Baby.” New England Journal of Medicine, 1995.
- Eliahu Levitas, MD et al. “Relationship between the duration of sexual abstinence and semen quality: analysis of 9,489 semen samples.” Fertility & Sterility, 2005.
- I Tur-Kaspa et al. “Semen characteristics in consecutive ejaculates with short abstinence in subfertile males.” Reproductive Biomedicine Online, 2016.
- Alison Taylor. “ABC of subfertility: Extent of the problem.” BMJ, 2003.
- Isiah D Harris, MD et al. “Fertility and the Aging Male.” Reviews in Urology, 2011.