When a couple faces challenges with conceiving the natural way, they may start to explore fertility treatment. In vitro fertilization (IVF) is a well-known fertility treatment that can help some people or couples become pregnant. Let’s discuss how the in vitro fertilization process works, in vitro fertilization success rates, in vitro fertilization costs, what the benefits are, and who is a good candidate for IVF.
Key takeaways
- In vitro fertilization (IVF) is a powerful fertility treatment that can treat infertility due to male or female factors.
- Many patients try IUI before moving on to IVF. The main differences between IVF and IUI are the procedures, effectiveness, and price.
- In vitro fertilization success rates vary based on the age and quality of the sperm and eggs, as well as the contributing factors to infertility. It’s generally considered the most effective option for creating a pregnancy with a couple’s own genetic material.
- IVF can be pricey — around $12,000 or more. Some health insurance may assist with in vitro fertilization costs.
What is in vitro fertilization?
In vitro fertilization (IVF) is an assisted reproductive technology (ART), a medical procedure used to help create a healthy pregnancy. During IVF, eggs and sperm are combined in a lab to promote fertilization. Then, the fertilized eggs — called embryos — can be tested, frozen, or implanted into the uterus to attempt pregnancy.
In vitro fertilization (IVF) is a powerful treatment with good success rates, but it can be expensive. Those facing challenges with fertility may try IVF if other methods have been unsuccessful.
A step-by-step guide to the in vitro fertilization process
An in vitro fertilization (IVF) cycle — AKA one treatment period — generally takes about 3 weeks. But, there’s also preparation that needs to happen prior to the cycle for maximum success. Let’s review what the IVF process looks like.

IVF step 1: Preparing for an IVF cycle
Before beginning IVF, both patients — the person who’s producing the sperm, and the person who’s producing the eggs — should do some necessary testing and prepare their bodies for treatment. While some factors, like genetics, are hard to avoid, implementing healthy lifestyle changes can improve in vitro fertilization success rates.
Important testing prior to in vitro fertilization (IVF) includes:
- STI testing and other infectious disease screening
- Semen analysis, to ensure sperm is healthy enough for IVF
- Ovarian reserve testing, to estimate how many eggs will be retrieved during the IVF cycle
Typically, in vitro fertilization (IVF) is planned as part of ongoing treatment with a reproductive endocrinologist (infertility specialist). Therefore, most people or couples planning for IVF will have already had a consultation and/or completed the above testing.
While some factors, like genetics, are hard to avoid, implementing healthy lifestyle changes can improve the chances of successful IVF treatment.
Prepping for IVF treatment can involve:
- Eating a healthy balanced diet
- Reaching or maintaining a healthy weight
- Avoiding smoking and drinking
- Taking vitamins, such as prenatal vitamins and/or male fertility supplements
If you’re planning to try IVF, your reproductive endocrinologist will let you know about anything else you should do in advance to maximize your chances of success.
Finally, you’ll make a plan of action for your cycle with your doctor. This will include deciding on your medication protocols, cycle timing, etc. Cycle timing will likely be based on the female patient’s natural menstrual cycle. If they have an irregular cycle or want to adjust the timing of their treatment, they may be on birth control pills for a period of time prior to their IVF treatment.
IVF step 2: Monitoring and ovarian stimulation
The “active” part of the IVF cycle begins on the first day of the female patient’s menstrual cycle, also known as “day 1.”
At this point, two things start: ovarian stimulation medication, and a series of appointments to track the progress of the medication, known as monitoring.
Controlled ovarian stimulation involves using injectable hormone medications that stimulate the ovaries to produce eggs. Typically, a person with ovaries will produce a single egg during a menstrual and ovulation cycle (or rarely, two). Ovarian stimulation helps improve in vitro fertilization success rates by increasing the number of eggs that are matured and released during one cycle.
Typically, ovarian stimulation medications are prescribed for 8–11 days. During that time, the patient will be expected to complete office visits for an ultrasound and bloodwork every 1–2 days. These visits, known as “monitoring” appointments, allow medical providers to keep track of how the medication is affecting the ovaries, to ensure a patient isn’t making too few — or too many — eggs.
IVF step 3: Egg retrieval and semen collection
Both the male partner/person providing sperm and the female partner/person providing eggs will have a role in this step of the in vitro fertilization (IVF) process.
The egg retrieval is the culmination of the ovarian stimulation process, performed when enough eggs are mature. During an egg retrieval, an outpatient surgical procedure, the patient is sedated. Using ultrasonography to guide their way, the doctor will carefully remove the eggs from the ovaries using a needle. The eggs go directly to the lab, and are cultured in an incubator until semen is collected.
The second part of this step is semen collection. The male patient will masturbate to produce a semen sample. In some cases, this process is done before egg retrieval, and sperm can be frozen for use during IVF.
IVF step 4: In vitro fertilization and embryo development
In this step, the sperm is combined with the cultured eggs. If the sperm count is high enough, the embryologist — or lab scientist — can simply place the eggs and the sperm in a lab dish, and allow them to fertilize naturally.
The fertilized eggs, or zygotes, are incubated and monitored for several days to ensure they enter the blastocyst stage. Blastocysts have over 100 cells and some distinct cell layers.
Once embryos reach the blastocyst stage, the embryologist and/or reproductive endocrinologist can assess the quality of the embryos, based on how much they’ve expanded and differentiated into sections and structures.
The grading system for embryo quality is as follows:
- Grade A: Embryos with excellent quality and high chances of successful implantation.
- Grade B: The quality of embryos are good, with a decent chance of implantation.
- Grade C: These embryos are considered average, with a lower chance of implantation.
- Grade D: Embryos with poor quality and probability of implantation.
Choosing embryos based on these characteristics can help select the most robust embryos with the highest chances of survival after implantation. However, this is not as accurate as preimplantation genetic testing when it comes to determining which embryos are most likely to result in a healthy pregnancy.
Optional step: ICSI
If the sperm count is low or sperm motility (AKA movement) is poor, a reproductive endocrinologist may recommend intracytoplasmic sperm injection (ICSI).
ICSI is an IVF technique in which a single sperm cell is inserted into the center (or nucleus) of the egg using a needle. This method was created to help increase the chances of fertilization for men with a low sperm count or motility, or those who have been unsuccessful with IVF, and may improve in vitro fertilization success rates.
IVF step 4: Embryo transfer, testing, and/or freezing
In most cases, embryos are transferred at the blastocyst stage, around day five. The transfer is a simple non-surgical procedure that does not require sedation or anesthesia. A doctor will load an embryo into a catheter that’s inserted through the female patient’s cervix and into the uterus, often using ultrasound to guide them. The doctor then uses the plunger at the end of the catheter to “flush” the embryo into the uterus, where it will hopefully implant and create a pregnancy.
In modern IVF cycles, the “gold standard” is to transfer one high-quality embryo at a time. If a patient or couple doesn’t have many high-quality embryos, the doctor may recommend transferring two at a time.
Optional step: Embryo freezing
Additional embryos can be frozen for future use. Embryo freezing, or cryopreservation, allows the option to attempt pregnancy again or have additional children.
If you need additional time to prepare to attempt pregnancy — if, for example, you have a thin uterine lining or have lingering side effects from your IVF cycle — you may also be advised to freeze all of your embryos and attempt your first embryo transfer after a month or so.
Optional step: Embryo genetic testing
Some patients or couples may choose to do genetic testing on their embryos at this point in the IVF process. Instead of immediately transferring the embryos, an embryologist can do an “embryo biopsy,” in which a small piece of tissue — just a few cells — is removed from the embryo for genetic testing.
Embryo genetic testing can tell your healthcare provider one of two things:
- Whether the embryo(s) have the proper number and arrangement of chromosomes, making them “euploid” (genetically healthy) and more likely to result in a healthy child
- Whether the embryo(s) contain certain genes or genetic mutations associated with a specific disease, such as cystic fibrosis, that the parents may carry
If embryo genetic testing is performed, the embryos will be frozen while they await the results of the testing. Then, you may thaw one or more embryos to attempt pregnancy in a future embryo transfer.
IVF step 5: hCG pregnancy blood test
The final step of an in vitro fertilization (IVF) cycle is a hormone chorionic gonadotropin (hCG) blood test two weeks post-embryo transfer. This test measures the amount of hCG or “pregnancy hormones” in the body.
Taking a pregnancy test early can result in a false positive, which is why healthcare providers recommend patients wait the entire two weeks. If the test is positive, the patient will take another test two days later to confirm the hCG levels are rising appropriately.
Who should consider in vitro fertilization (IVF)?
In vitro fertilization (IVF) is a good choice for:
- People with blocked fallopian tubes.
- People with advanced endometriosis.
- People with moderate to severe male-factor infertility.
- People using sperm retrieved directly from the testes.
- People with limited amounts of frozen sperm and no “fresh” sperm option.
- People who want to or need to do genetic testing on their embryos (such as couples who carry certain genetic illnesses).
- People who have tried multiple IUI cycles without success.
Is in vitro fertilization (IVF) a good choice for male-factor infertility?
In vitro fertilization, especially with the addition of intracytoplasmic sperm injection (ICSI), can be a powerful treatment for those dealing with male-factor infertility. IVF without ICSI is generally an option for those with a total motile sperm count of 5 million or more. IVF with ICSI requires only a single sperm per egg, so can be used even when sperm is scarce or has very low or no motility.
Not sure what your total motile sperm count is? We offer at-home semen analysis kits that test male fertility, including sperm concentration, sperm volume, sperm motility, sperm morphology, and total motile sperm count, giving you and your medical team a picture of your likelihood to conceive with IUI. Learn more about how at-home sperm testing works.
If you receive abnormal semen analysis results, those results may be used to give you a male-factor infertility diagnosis. You can talk to your doctor or a urologist about ways to improve your sperm health and improve your chances of success with intrauterine insemination (IUI) or other fertility journeys.
Should I do sperm freezing before in vitro fertilization?
Many couples or patients choose to do sperm freezing prior to IVF. Freezing sperm prior to fertility treatment ensures that you have a back-up plan for your in vitro fertilization (IVF) cycle. If you have frozen sperm, you can have a successful IVF cycle even if the male patient cannot produce a sample on the day of the egg retrieval, or if the sample produced doesn’t have enough motile sperm.
Using frozen sperm for IVF won’t affect won’t affect the in vitro fertilization process. Studies demonstrate that frozen sperm is equally as successful as “fresh,” never-frozen sperm when used in IVF cycles. Learn more about sperm freezing.
Legacy offers a sperm testing and freezing kit, which saves a trip to a sperm bank or fertility clinic. Learn more about how at-home sperm freezing works.
In vitro fertilization success rates
In vitro fertilization success rates vary depending on the age of the biological parents. According to the CDC, in vitro fertilization success rates are as follows:
| Age of person trying to get pregnant | Chance of live birth per IVF egg retrieval |
| Under 35 | 55.7% |
| 35–37 | 41.5% |
| 38–40 | 27.6% |
| Over 40 | 9.5% |
The age of the sperm also plays an essential role in in vitro fertilization success rate. Older sperm can affect in vitro fertilization success rates, even when the female partner is younger. In fact, a 2022 study found that paternal age over 40 years old was associated with a significantly lower chance of live birth when using IVF.
| Age of male partner | Live birth rate per embryo transfer |
| ≤ 39 years old | 39.1% |
| 40–44 years old | 25.9% |
| 45–50 years old | 23.0% |
| 51–55 years old | 22.9% |
A 2019 study revealed that frozen embryo transfer (FET) could increase in vitro fertilization success rates, especially for those doing IVF for male-factor infertility. Of 453 couples, 298 had a fresh embryo transfer, and the remaining 155 patients had FET. Patients with FET had a higher in vitro fertilization success rate of 60.70%, compared to 49.32% for the new embryo group.
This is likely due to the fact that those who freeze embryos can take a break between their egg retrieval and their embryo transfer, to fully prepare their uterus to optimally receive an embryo. It’s also possible, researchers theorize, that freezing and thawing embryos inherently selects for healthier embryos, as less healthy ones may not survive the process.
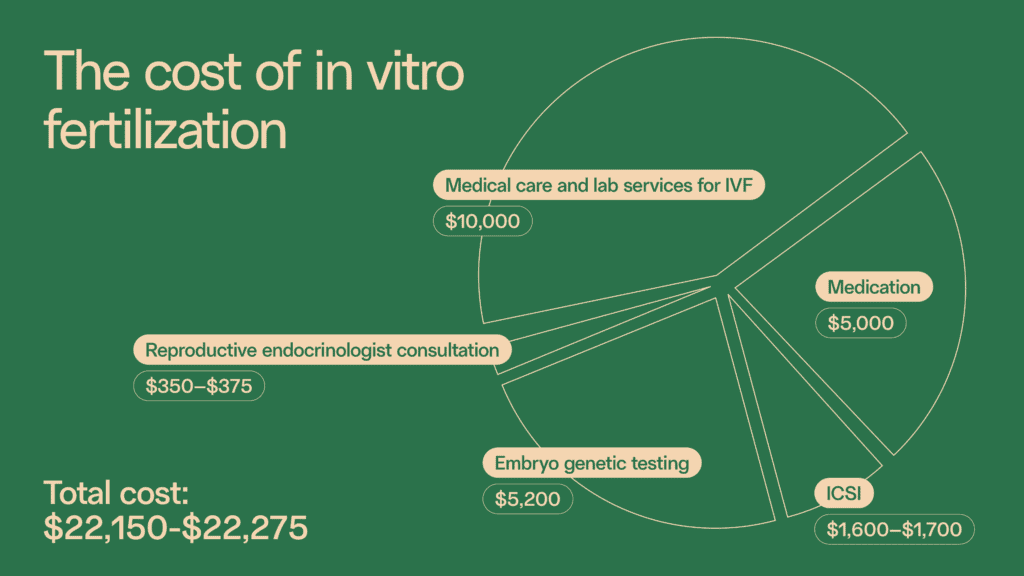
In vitro fertilization cost
As mentioned earlier, IVF can be a pricey fertility treatment. In vitro fertilization costs for a single IVF treatment can range between $12,000 and $30,000. Factors that affect in vitro fertilization costs include where the treatment happens and any medications or additional services, like ICSI or embryo genetic testing, the hopeful parents may need.
FertilityIQ breaks down average in vitro fertilization costs as follows:
- Reproductive endocrinologist consultation: $350–$375
- Medical care and lab services for IVF: $10,000
- Medication: $5,000
- ICSI: $1,600–$1,700
- Embryo genetic testing: $5,200
Does health insurance cover in vitro fertilization (IVF)?
In some US states, and in some cases, health insurance will cover some or all of the in vitro fertilization process and in vitro fertilization costs.
Some US states have fertility insurance coverage “mandates,” which means that certain insurance plans are required to cover treatments like in vitro fertilization (IVF) and reduce in vitro fertilization costs. In other places, employers may opt for more comprehensive insurance plans that include infertility services, or may contract separate fertility benefits, such as Carrot, Progyny, or WINFertility.
In order to receive coverage for in vitro fertilization (IVF), patients will typically need a diagnosis of infertility. Many insurance plans also require the patient to try intrauterine insemination (IUI) first.
Patients should always check with their health insurance provider to see if in vitro fertilization costs can be reduced or fully covered under their plan.
What is the difference between intrauterine insemination (IUI) and in vitro fertilization (IVF)?
While both are artificial fertility treatments that improve the chances of pregnancy, their processes differ quite significantly. IUI is less invasive, but also less effective, than IVF.
Learn more about intrauterine insemination (IUI).
IVF vs. IUI: Process
During intrauterine insemination (IUI), sperm is injected directly into the uterus at the time of ovulation. This can help facilitate fertilization by giving sperm a “kickstart” on its journey to the egg. IUI can be helpful for patients with ovulatory issues or mild to moderate male-factor infertility.
IVF vs. IUI: Cost
IUI is more affordable than IVF, with prices starting around $500, while in vitro fertilization costs can be upwards of $10,000 or more.
According to FertilityIQ, here’s a breakdown of what intrauterine insemination costs:
- In-office intrauterine insemination cost: $400
- Pre-IUI monitoring: $500–$1,000
- Medications: $150–$1,000
IVF vs. IUI: Success rates
As described above, IVF is one of the most powerful fertility treatments, with in vitro fertilization success rates around 40–50% for many patients. IUI is generally considered less effective.
The average intrauterine insemination success rate is approximately 10% per cycle for those who don’t use ovulation medication, and about 15–25% for those who do. Cumulative cycles can increase overall intrauterine insemination success rates. Most pregnancies occur within the first four IUI cycles.
Because IUI is less expensive and invasive than IVF, many patients will try IUI first, for perhaps 3–6 cycles, before moving on to IVF.