There are many potential causes that can lead to an infertility diagnosis. One is azoospermia, a condition in which there are no sperm in the semen — this can have obstructive or nonobstructive causes. Sertoli cell-only syndrome or “SCO syndrome,” a rare condition estimated to affect less than 5–10% of infertile men, is a non-obstructive cause of azoospermia and male infertility.
If you suspect that you have Sertoli cell-only syndrome or have been recently diagnosed, that doesn’t mean you’re left without any options to start a family. There are reproductive assistance technologies that you can consider, and using a sperm donor is another option too.
To learn more about the symptoms of Sertoli cell-only syndrome, the diagnosis process, and the chances of pregnancy with Sertoli cell-only syndrome, read on.
Key takeaways
- Sertoli cell-only syndrome is a condition in which the testicles don’t produce sperm properly.
- Most people with Sertoli cell-only syndrome won’t know until they do fertility testing.
- Testicular sperm extraction and ICSI may be able to help some with SCO have a genetic child.
What are Sertoli cells?
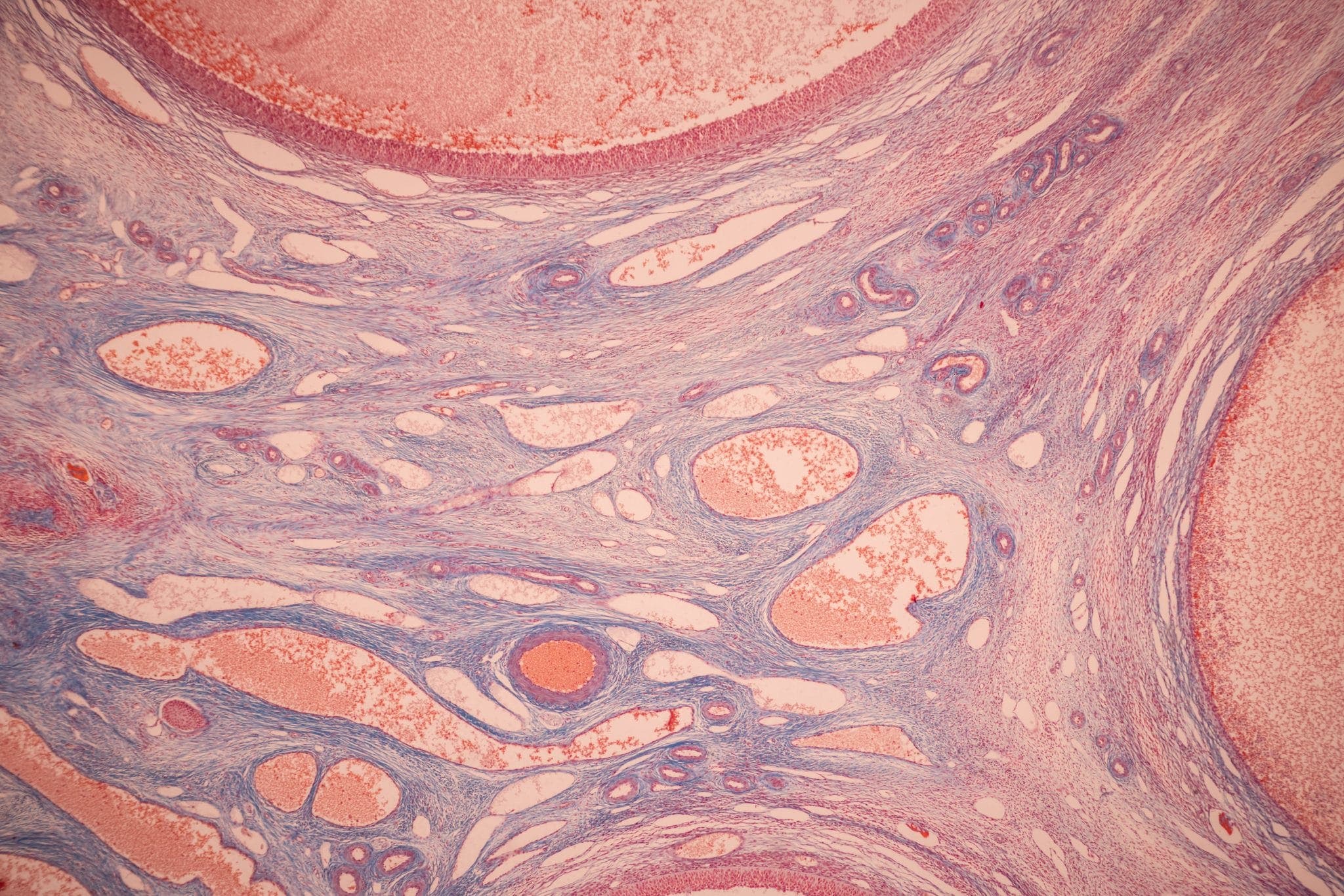
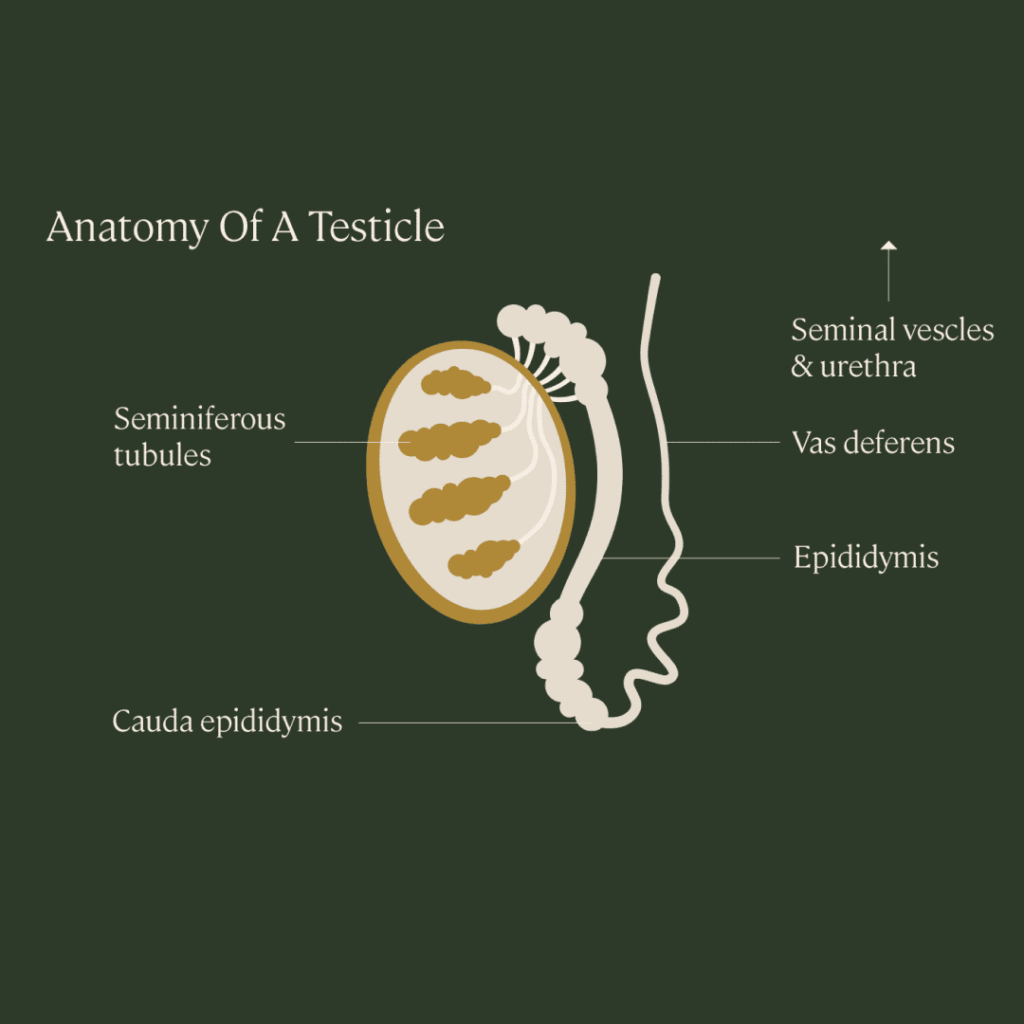
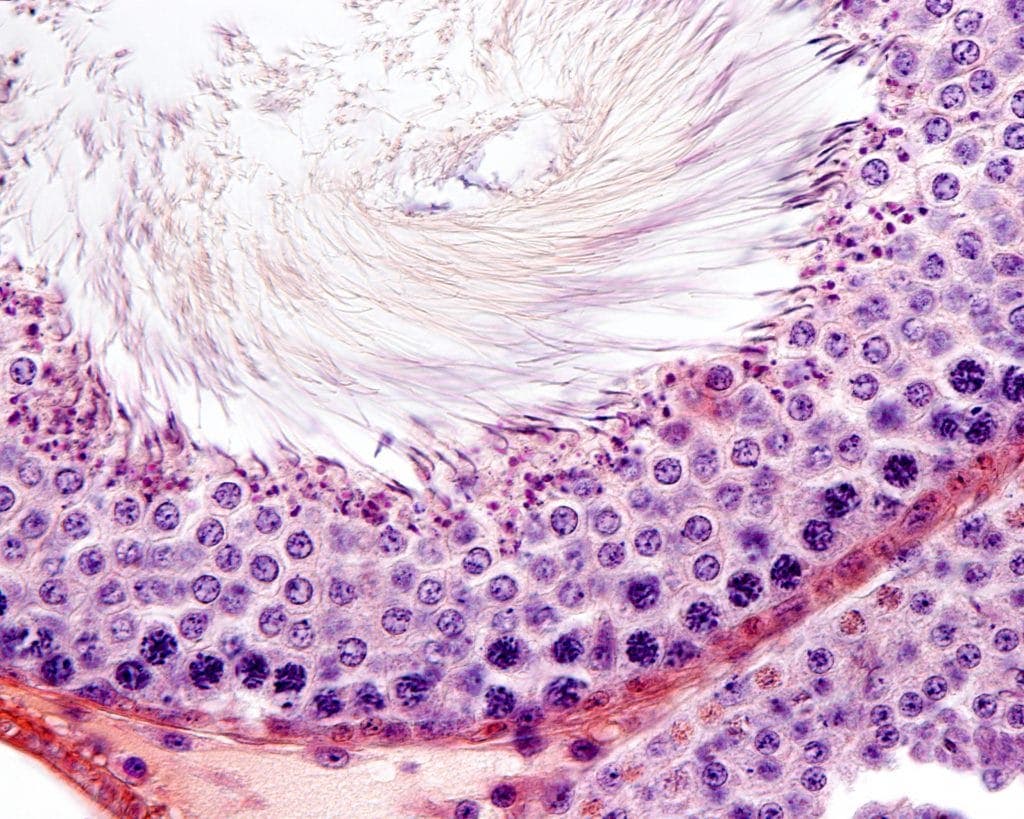
Sertoli cells are cells in the testicles that assist in the process of sperm production (known as spermatogenesis). They’re located in the wall of the seminiferous tubules, the structure in the testicles where sperm are produced. Also called “nurse” cells, Sertoli cells provide nutrition and hormonal support to developing sperm, and clean up excess cell parts during the sperm production process.
In healthy testicles, the seminiferous tubules are filled with sperm in various stages of cell division and maturation, along with Sertoli cells.
What is Sertoli cell-only syndrome?
Sertoli cell-only syndrome, also known as Del Castillo syndrome or germ cell aplasia, is a condition in which the seminiferous tubules contain only Sertoli cells, with very low numbers of sperm or no sperm cells present.
Patients with Sertoli cell-only syndrome are often diagnosed with azoospermia, a condition characterized by the absence of sperm found in ejaculated semen, and with infertility.
SCO syndrome patients also typically have higher levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) in their blood. High levels of FSH typically indicate that the testicles are not functioning properly. Normal FSH levels in adult males are typically between 1.5 to 12.4 mIU/mL.
Symptoms of Sertoli cell-only syndrome
In most cases, a person won’t realize or suspect they have Sertoli cell-only syndrome until they have difficulty trying to conceive. Typically, people with Sertoli cell-only syndrome have normal sexual function and ejaculation without any glaring warning signs.
In some cases, it’s been found that people with Sertoli cell-only syndrome may have small testicles. According to the Human Phenotype Ontology, a set of data about physical abnormalities collected by clinicians, Sertoli cell-only syndrome has been associated with:
- Abnormality of the chest
- Enlarged male breast (called gynecomastia)
- Obesity
- Metabolic abnormalities
Again, most patients with Sertoli cell-only syndrome do not experience symptoms. Lab tests are usually performed when a couple is having trouble conceiving, which can lead to a diagnosis.
How is Sertoli cell-only syndrome diagnosed?
When a couple is having trouble conceiving, the frontline test for the sperm-producing partner is a semen analysis. For this test, the patient must produce a semen sample, which is analyzed for multiple sperm quality parameters. This includes semen volume and sperm count/concentration (how many sperm), motility (how well sperm are swimming), and morphology (the size and shape of sperm).
If the test results come back with abnormally low sperm count and concentration, then your physician will likely order a second analysis to confirm the findings. If it’s confirmed that you have zero or virtually zero sperm count, then you may be diagnosed with azoospermia.
Understand the difference between cryptozoospermia and azoospermia.
From there, it’s probable that your physician will order additional diagnostic tests to understand what may be causing the azoospermia. This can include imaging to search for any obstructive causes or blood tests to check for hormonal or genetic causes.
For Sertoli cell-only syndrome, tests that confirm the diagnosis include:
- Blood work that shows increased FSH levels, with or without high LH or low testosterone (low testosterone may indicate Klinefelter syndrome, a genetic cause for male infertility)
- A biopsy of the testicles, demonstrating very few or no sperm cells inside the seminiferous tubules
Causes of Sertoli cell-only syndrome
Most cases of Sertoli cell-only syndrome are idiopathic, meaning the cause is unknown. However, that’s not the case for all patients. Based on current research, there are a few potential causes of Sertoli cell-only syndrome, which include:
- Genetic factors or inheritance by a genetic mutation, such as:
- Klinefelter syndrome (also known as “47 XXY”), a chromosomal condition in which a biological male is born with an additional copy of an X chromosome
- Y-chromosome microdeletions (YCM), a family of genetic disorders caused by missing genes in the Y-chromosome
- Hormonal factors
- Toxin exposure
- History of exposure to radiation
- History of trauma to the testicular region
- History of a viral infection affecting the testicles
In one study, it was found that karyotype (genetic) abnormalities were the most common abnormality seen in Caucasian azoospermic people with Sertoli cell-only syndrome.
Treatments for Sertoli cell-only syndrome
At the moment, there are no reliable treatment methods for people diagnosed with Sertoli cell-only syndrome. Aside from difficulty or inability to have biological children, most people with Sertoli cell-only syndrome do not experience other side effects or health concerns related to the syndrome.
What are the chances of pregnancy with Sertoli cell-only syndrome?
Although most people with Sertoli cell-only syndrome do not produce sperm, some people with Sertoli cell-only syndrome are able to make a few sperm. This can typically be identified during a testicular biopsy. If so, doctors may be able to use testicular sperm extraction (TESE), a procedure to remove sperm directly from the testicles, to obtain a few sperm. Then, that sperm can be used with intracytoplasmic sperm injection (ICSI), an IVF technique in which a single sperm is injected directly into an egg.
Success rates for this procedure are on the low side — around 13% — for people with nonobstructive azoospermia, including SCO syndrome. In one study, a group of 148 men with Sertoli cell-only syndrome underwent TESE and ICSI; sperm was successfully retrieved in 35 cases (about 24%) and pregnancy was achieved in 4 cases (about 3%).
In another study, sperm retrieval rates were higher, with sperm being found in 45% of patients using TESE. Pregnancy rates in this study were higher, as well: 134 of the 290 who were able to retrieve sperm achieved a pregnancy, for a total pregnancy rate of around 21%.
For those unable to produce any sperm, choosing to use donor sperm is another option, as well as pursuing adoption.
Is Sertoli cell-only syndrome genetic or inherited?
Emerging research suggests that Sertoli cell-only syndrome is linked to some genetic conditions, including Klinefelter syndrome and Y-chromosome microdeletions.
If you’ve been diagnosed with SCO syndrome and plan to try for genetic children, discuss with your physician the likelihood of passing on this condition. Since genetic mutations that cause Sertoli cell-only syndrome occur within the Y-chromosome, the syndrome can only potentially be passed on to male offspring.
Understand your fertility: start with a semen analysis
If you are experiencing difficulty conceiving but do not yet understand why, starting with a semen analysis can help you get the answers you need. With at-home semen analysis kits offered by Legacy, you get lab reports in an easy-to-understand format and a consultation with a fertility specialist to go over your results and figure out the next steps. To learn more about what to expect from a semen analysis, you can check out our sperm testing guide here.