Cryptozoospermia is a term for semen with an extremely low concentration of sperm. With cryptozoospermia, the sperm count is so low that it may even be measured as zero in an initial analysis. This low concentration impacts fertility, making it difficult to conceive naturally. We’ll examine the causes of cryptozoospermia, how it’s treated, and how it affects your fertility.
Key takeaways:
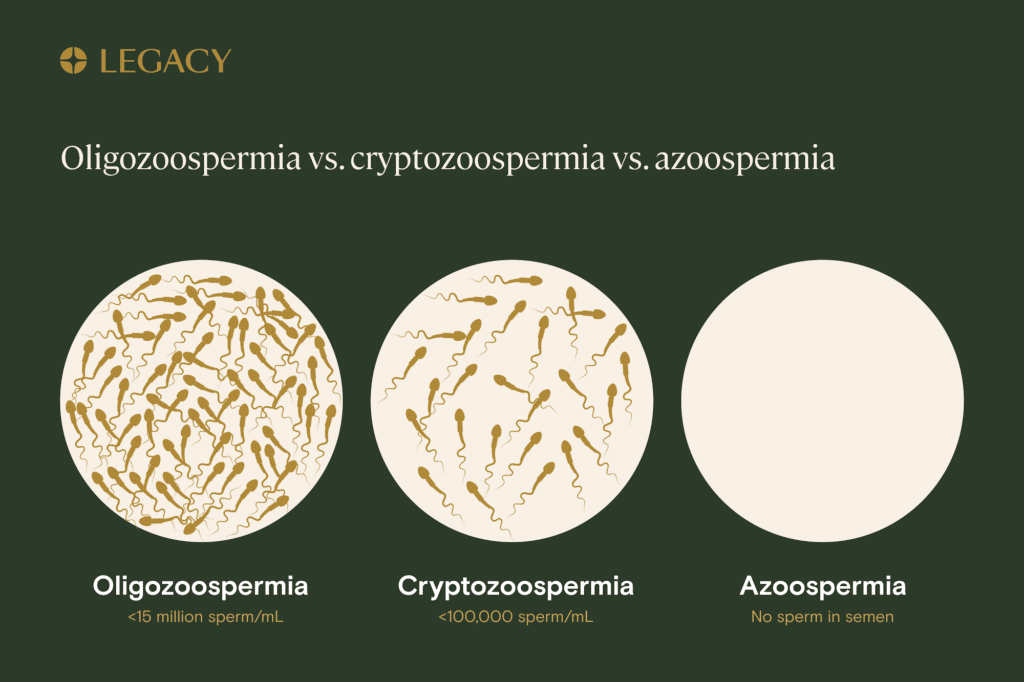
- You may be diagnosed with cryptozoospermia if your semen contains an extremely low number of sperm. It’s different from oligozoospermia or oligospermia (low sperm count) and azoospermia (no sperm in the semen at all).
- Cryptozoospermia can be caused by genetics or certain medical conditions, and may be influenced by lifestyle. The cause will determine whether and how it can be treated.
- Assisted reproductive technology can help people with cryptozoospermia conceive a child.
What is cryptozoospermia?
Cryptozoospermia is defined as a sperm concentration of less than 100,000 sperm per milliliter of semen. Often, the sperm count may be initially measured as zero, causing the condition to be known as “virtual azoospermia.” Sperm may then be found after the semen is put through a centrifuge and examined through a microscope.
One study of men at infertility clinics in Turkey indicated that cryptozoospermia was found in 27.2% of male-factor infertility cases. However, it noted that the prevalence varied based on patients’ backgrounds, including their genetics, age, lifestyle, and region.
Cryptozoospermia vs. oligozoospermia or azoospermia
Cryptozoospermia, oligozoospermia (also known as oligospermia), and azoospermia each refer to varying degrees of low or no sperm counts. Often, patients diagnosed with cryptozoospermia or oligospermia also have abnormal sperm motility (movement, a measure of how well sperm “swim”) and morphology (shape, size, and structure).
Oligozoospermia is diagnosed when semen has a low sperm concentration of less than 15 million sperm per milliliter of semen. Specifically:
- Mild oligospermia is 10–15 million sperm/mL.
- Moderate oligospermia is 5–10 million sperm/mL.
- Severe oligospermia is 0–5 million sperm/mL.
This is higher than cryptozoospermia, which is marked by a very low concentration of sperm in the semen of less than 100,000 per milliliter.
Finally, azoospermia is a condition in which there’s a complete absence of sperm in the semen. Azoospermia occurs in up to 20% of male-factor infertility cases and around 1% of the male population as a whole.
While assisted reproductive techniques are typically needed for those with azoospermia and cryptozoospermia, people with oligozoospermia can often still conceive naturally. In fact, 5% of fertile men have oligozoospermia.
These definitions sometimes come close to overlapping and may be hard to distinguish. One study noted that andrologists (male fertility and sperm health experts) sometimes have difficulty diagnosing cryptozoospermia versus severe oligozoospermia. Plus, sperm counts can change over time — a study of 208 men found that 24.6% of those with severe oligozoospermia eventually progressed to azoospermia.
What causes cryptozoospermia?
Several factors can cause cryptozoospermia, including genetics, medical conditions, and lifestyle.

Genetic causes for cryptozoospermia
One study of 997 patients with cryptozoospermia and azoospermia found that 28.4% had chromosomal abnormalities. One of the most common abnormalities found was a condition known as Klinefelter syndrome, in which a patient has an extra X chromosome. Klinefelter syndrome leads to infertility.
Research shows that Y chromosome microdeletion, a condition in which a patient is missing segments of DNA in the azoospermia factor (AZF) region of the Y chromosome, is also seen in people with cryptozoospermia. Since genes on the Y chromosome regulate sperm production, altering or deleting them can impact fertility.
A recent case study of a cryptozoospermic patient also identified a mutation in the TEX15 gene, a gene that codes for specific proteins, resulting in an altered protein that plays a role in fertility. The mutation may occur in people whose parents are genetically related, and may negatively affect sperm production, leading to cryptozoospermia or azoospermia.
Medical causes for cryptozoospermia
Medical conditions that can reduce sperm counts and cause cryptozoospermia include:
- Hypogonadism, in which the testes produce insufficient testosterone.
- Varicocele, or abnormally enlarged veins in the scrotum. Varicocele causes increased temperature in the scrotum, which can impact sperm production and result in cryptozoospermia, along with heightened oxidative stress and other factors that negatively affect sperm quality.
- Undescended testicle(s).
- Testicular cancer.
- Overweight and obesity, which were linked to increased rates of low sperm counts and azoospermia in a 2012 meta-analysis.
Lifestyle factors can contribute to cryptozoospermia, too. One case report found that chronic alcohol use led to cryptozoospermia and then azoospermia. Cigarette smoking may also contribute to cryptozoospermia.
How is cryptozoospermia diagnosed?
Cryptozoospermia is diagnosed based on the concentration of sperm in your semen, assessed during a semen analysis. A semen analysis is a test in which a sample of semen, produced via masturbation, is examined under a high-powered microscope to determine sperm count/concentration, motility, and morphology. (Legacy offers the option for a clinic-grade semen analysis without leaving home.)
You are considered cryptozoospermic if a semen analysis finds less than 100,000 sperm per milliliter of ejaculated semen. If you have a very low sperm count, your semen can be put through a centrifuge (a device that spins the sample to separate sperm from seminal fluid) and microscopically analyzed to detect sperm and make the diagnosis, a process known as sperm pellet analysis. Since semen parameters can vary, it’s recommended that you get multiple analyses to confirm the diagnosis.
Treatment for cryptozoospermia
The treatment for cryptozoospermia depends on its cause.
For cryptozoospermia caused by varicocele, surgical repair may offer a solution. One small study of 14 virtually azoospermic (cryptozoospermic) men found that surgically repairing the varicocele improved semen parameters in 85.7%, and led to three subjects conceiving children.
A common treatment for hypogonadism, testosterone replacement therapy, is not effective for cryptozoospermia because testosterone can further limit sperm production. For those with secondary hypogonadism (hypogonadism that’s caused by issues in the hypothalamus or the pituitary gland), human chorionic gonadotrophin (hCG) therapy may help improve the condition without further impairing sperm production.
If you have an undescended testicle, surgery to move the testes into the scrotum may increase sperm counts. While this is typically only effective when done at a young age, one case report of an azoospermic man found that the surgery restored sperm production at the age of 26; within two months after the operation, the patient’s semen showed cryptozoospermia, with further improvements after six months.
Finally, lifestyle changes may help. The aforementioned case study of cryptozoospermia and eventual azoospermia caused by alcohol reported that the patient regained normal semen parameters within three months of drinking cessation. For people with obesity, losing weight may improve sperm parameters, though recent research notes that more studies are needed.
Can people with cryptozoospermia achieve a natural pregnancy?
It’s unlikely you’ll be able to conceive naturally if you have cryptozoospermia. This is because the extremely low sperm count, which is typically seen alongside reduced motility, impairs fertility. In most cases, assisted reproductive technology is needed.
Fertility treatment options for cryptozoospermia

People with cryptozoospermia may use intracytoplasmic sperm injection (ICSI) to achieve a pregnancy. ICSI is an IVF procedure that involves injecting a single sperm directly into an egg. ICSI is different from conventional in vitro fertilization (IVF), where sperm placed in a dish with an egg can penetrate and fertilize it on its own. ICSI may be helpful in cases of severe male-factor infertility, such as cryptozoospermia, where there are very few sperm in the semen.
If sperm is difficult to find in the ejaculated semen, it may need to be extracted directly from the testicles in a process known as TESE (testicular sperm extraction) or TESA (testicular sperm aspiration). This can be helpful in cases where sperm is damaged as it moves through the reproductive tract. Some research indicates that testicular sperm contributes to a higher pregnancy rate and greater number of high-quality embryos compared to ejaculated sperm for patients with cryptozoospermia. Age may make a difference; one study indicates that ejaculated sperm achieves a higher birth rate for men under 35, while testicular may be a better option for older men.



