Although an infertility diagnosis can be discouraging, a number of sperm-boosting drugs and supplements can help improve male fertility issues. Find out what these medications and supplements are and learn more about what causes male-factor infertility in the first place.
Key takeaways
- Possible causes of male-factor infertility include low or no sperm count, poor sperm motility, and sexual or ejaculatory dysfunction.
- Medicine for improving sperm count or quality include Clomid, FSH, anastrozole, and hCG. These drugs should only be used by men diagnosed with infertility under the care of a physician.
- Supplements that are available without a prescription, including antioxidants, vitamin D, L-carnitine, folate, zinc, and D-aspartic acid, may also help improve sperm health and support healthy sperm production.
What are the causes of male-factor infertility?
Infertility affects one in six couples who are trying to conceive — and in at least half of all cases of infertility, a male factor is a contributing cause. This means that in the US, around 10% of all males who are attempting to conceive suffer from infertility.
Male fertility relies on a complex system of processes, including the ability to make healthy sperm, obtain an erection, and ejaculate to ensure the sperm reaches the egg. Problems with any of these processes may contribute to male-factor infertility.
Infertility may be diagnosed after a heterosexual couple has been actively trying to conceive for 6–12 months or more. In males, potential causes for infertility include low or no sperm count, poor sperm motility, and sexual or ejaculatory dysfunction.
Low or no sperm count
According to the World Health Organization (WHO), a normal sperm concentration is around 15 million sperm per milliliter (mL) of semen.1 When someone has a low sperm count, also known as oligospermia, the condition can have an adverse effect on fertility by reducing the chances of fertilizing the egg. Oligospermia doesn’t necessarily mean that you can’t conceive, but it does mean that your chances of conception are lower than those with higher sperm counts.
A 2006 study that looked at oligozoospermic couples found that those with a sperm concentration of over 2 million sperm per mL of semen had a 22.1% chance of natural conception. In cases where sperm count was less than 2 million per mL of semen, chances of natural conception dropped to 1.6%.2
Cryptozoospermia refers to an extremely low concentration of sperm (less than 100,000 sperm per mL of semen). In some cases, the sperm count may be measured as zero in an initial analysis. In one 2018 study of men at infertility clinics in Turkey, cryptozoospermia was found in 27.2% of male-factor infertility cases.3
A complete absence of sperm is called azoospermia. This condition is experienced by 15% of those with male-factor infertility and 1% of the general male population.4 Because there is no sperm present in semen, azoospermia makes conception without medical intervention improbable.
Poor sperm motility
Sperm motility is sperm’s ability to move and “swim.” Poor sperm motility, or a low number of sperm swimming efficiently, is another factor that can lead to fertility issues.
A healthy semen sample has at least 40% motile sperm, and has at least 32% progressive motility5 — meaning that the sperm are not just moving, but moving in straight lines or large circles, paths that help the sperm reach and fertilize an egg. Various studies indicate statistically significant decreases in motility of 0.6% per year of age, resulting in a 3–12% decline in motility over 20 years.6
Read more about how to improve sperm quality and motility.
Sexual or ejaculatory dysfunction
Sexual dysfunction, including reduced sexual desire and erectile dysfunction, may cause fertility issues by making sexual intercourse more difficult. The chances of developing erectile dysfunction increase with age due to lower testosterone levels and restricted blood flow, but age is not the only cause. A 2024 study found that 24% of American men experienced erectile dysfunction, and the prevalence increases with age.7
During ejaculatory dysfunction — which may include premature ejaculations, retrograde ejaculation, or delayed ejaculation — sperm may not effectively reach the female reproductive system, which can negatively impact fertility. The prevalence of male infertility due to ejaculatory dysfunctions is overall just under 2%.8

Medications to improve sperm production
Some causes of male-factor infertility, such as low sperm count or poor sperm quality, may be treatable with medication. Remember, these medications should only be used by men diagnosed with infertility under the care of a physician.
The most common sperm improvement medications include:
Clomid (clomiphene citrate) for male infertility
Though Clomid (clomiphene citrate) is typically used to treat female infertility, it may also help in cases of low sperm count or quality. Clomid is an estrogen modulator, meaning it blocks estrogen from interacting with the pituitary gland. This can increase the levels of other male fertility hormones, including
Clomid has been shown to increase sperm concentration and motility, which could help oligospermic or poor motility patients achieve pregnancy.9
For azoospermic patients, Clomid may resume sperm production or increase the odds of a successful testicular sperm extraction, in which sperm cells are retrieved via needle directly from the testes and then transferred to a lab to mature.
In a study of 42 azoospermic patients given clomiphene citrate, 64.3% of the patients had sperm in their semen analyses post-treatment (ranging from 1 to 16 million sperm/mL with an average concentration of 3.8 million/mL). Sufficient sperm for intracytoplasmic sperm injection (ICSI) was retrieved via testicular sperm extraction in all patients, even though 35.7% remained azoospermic.10
FSH for male infertility
Follicle-stimulating hormone (FSH) is a hormone released by the pituitary gland in the brain. In males, it stimulates testicular growth and helps aid the creation of sperm cells. Across 17 clinical trials evaluating FSH use in infertile men, FSH was shown to increase overall pregnancy rates, especially in men with oligozoospermia, oligoasthenoteratozoospermia or OAT — in which all semen parameters are abnormal— and hypogonadism (low testosterone).11
FSH is typically an injectable hormone medication sold under the brand names Follistim and Gonal-F. Unfortunately, FSH is not effective for those with testicular failure, in which the testes cannot produce sperm even with proper levels of LH, FSH, and testosterone.
Anastrozole or letrozole for male infertility
Anastrozole and letrozole are medications that work to decrease the production of estrogen and increase testosterone in the body. Both have been shown to help correct hormonal imbalances and improve sperm production in men with subfertility.
In a 2017 study, 86 men with low T were treated with 1mg of anastrozole daily; 95.3% of patients had an increased serum T and decreased serum E2 after treatment, and sperm concentration and total motile counts improved in 18 of 21 men.12 Letrozole has similarly been shown to improve testosterone-to-estrogen ratios and semen parameters in infertile men.13
Testosterone replacement therapy for sperm production?
If a man has low testosterone levels that are contributing to infertility, why not just take injectable testosterone?
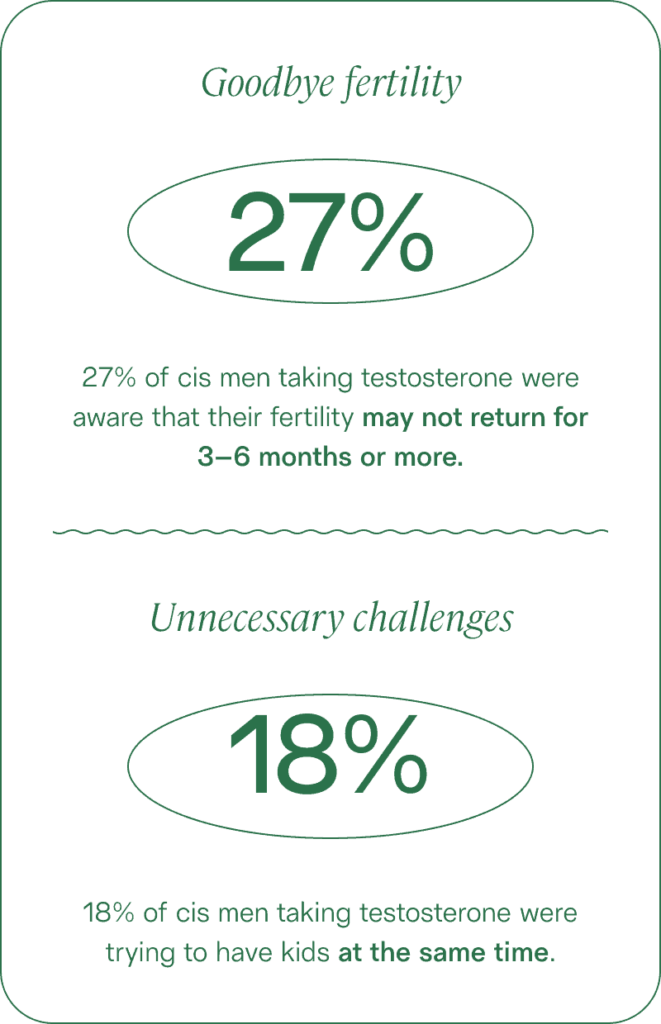
The use of exogenous (or external) testosterone, known as testosterone replacement therapy, seems like it would be beneficial for fertility. After all, a small amount of testosterone is necessary for the production of healthy sperm. And in fact, in a 2023 survey published by Legacy, 72% of respondents believed taking testosterone would improve a person’s fertility.
However, adding testosterone to the body disrupts the hypothalamic-pituitary-gonadal axis, the balance and flow of hormones from one part of the endocrine system to another. Exogenous testosterone actually works to inhibit the production of other fertility hormones, significantly impairing or even halting sperm production altogether.
In most cases, men taking testosterone will have zero sperm count within 4–6 months of starting therapy. TRT should not be undertaken by those who hope to conceive. Check out our guide to testosterone replacement therapy.
hCG for male infertility
Human chorionic gonadotropin (hCG) is actually a hormone primarily produced by the placenta during pregnancy — if you or your partner have ever used a pregnancy test “pee stick,” it’s hCG that the test is measuring in your urine. However, hCG also functions much like LH does in the body.
Treatment with hCG may help improve the condition of low testosterone (hypogonadism) caused by issues in the hypothalamus or the pituitary gland. According to a 2021 literature review spanning over 40 years of research, hCG therapy is considered the top choice for patients suffering from secondary hypogonadism because it triggers the body to produce testosterone and sperm without side effects on fertility, such as those seen in testosterone replacement therapy.14

Best supplements for male fertility
A number of male fertility supplements and over-the-counter “sperm booster” pills are available. From antioxidants like vitamin C and CoQ10 to amino acids and minerals, each of these supplements may help enhance sperm health and production. Here is what the research has to say about the efficacy of these supplements.
Antioxidants for male fertility
Studies show that high levels of oxidative stress in the body may result in damage to sperm DNA, potentially leading to male infertility and recurrent pregnancy loss.15 Antioxidants protect sperm and other cells from oxidative stress. Therefore, a diet high in antioxidants or antioxidant supplementation may improve male fertility.
- Vitamin C is one such powerful antioxidant. One 2006 study found that taking 1,000mg supplements twice a day for two months was associated with doubled sperm counts and a 90% increase in motility.16
- Vitamin E is another antioxidant that protects sperm, especially when combined with other antioxidants. A 2022 meta-analysis of studies found that vitamin E supplementation increased sperm count and, after six months, sperm forward motility.17 Another meta-analysis found that taking vitamin E with vitamin C “significantly improved” sperm count, concentration, motility, morphology, and pregnancy rate compared to a control group.18
- Coenzyme Q10, or CoQ10, is an antioxidant that may also improve sperm concentration, motility, and morphology. In one 2015 study, 60 men were treated with 150mg of CoQ10 daily. After 6 months of supplementation, sperm count was increased by 53%, along with significant improvement in sperm motility.19
- Selenium is a powerful trace mineral with antioxidant properties that can positively affect male fertility. One 2018 study found that infertile men who were prescribed 50 micrograms of selenium once a day for three months saw a noticeable increase in sperm count, motility, vitality, and morphology.20 Their levels of MDA — a marker of oxidative stress — also significantly decreased. The subjects also had an increase in testosterone and glutathione levels, both of which might also benefit male fertility.
- Lycopene is another powerful fertility-boosting antioxidant. A 2023 review of studies found that lycopene supplementation was associated with decreased oxidative stress and sperm DNA damage and increased sperm count, concentration, motility, and morphology.21
Vitamin D for male fertility
Vitamin D is a hormone responsible for regulating our body’s absorption of key minerals like calcium, magnesium, and phosphate. But several studies show it may also play a role in male fertility. A 2024 study found that having a low vitamin D level boosted men’s chances of asthenozoospermia (low motility) by 500%.22
In a 2020 study, vitamin D supplementation was associated with improved motility for men with asthenozoospermia.23 In another study, infertile men treated with vitamin D experienced an increase in sperm motility as well as a significantly higher number of pregnancies.24
Learn more about vitamin D and male fertility.
L-carnitine for male fertility
Derived from amino acids, L-carnitine is normally concentrated in the testis and epididymis. A 2023 review of studies found that supplementing with L-carnitine enhances sperm parameters, regulates hormone levels, reduces oxidative stress, and improves fertility rates, even at doses as low as 2g/day.25
Folate for male fertility
Also known as folic acid, folate plays a key role in reproductive health, namely sperm production. A 2017 review that looked at seven separate studies found a correlation between folate supplementation and increased sperm concentrations in men with fertility issues.26 Even more, subjects who combined folate with zinc showed improved sperm morphology as well.
Zinc for male fertility
Zinc is a nutrient that helps the immune system function and also plays a vital role in reproductive processes. Several studies show that zinc supplementation has been associated with a significant increase in semen volume, sperm motility, and normal sperm morphology, especially when combined with folate.27
D-aspartic acid
An amino acid that is concentrated in the testicles and sperm cells, D-aspartic acid (D-AA) is also used as a male fertility supplement, as it appears to have a role in regulating the release and synthesis of testosterone. One study found that D-AA for supplementation over the course of 90 days significantly increased the concentration and motility of sperm, nearly doubling concentration and boosting motility by over 50%.28 This resulted in an increased rate of pregnancies. D-AA acid may also work in combination with other supplements: A 2025 study found that infertile men who took D-AA with ubiquinol (CoQ10) and zinc for three months had significantly improved sperm motility and testosterone levels.29
Adopting healthy lifestyle habits, including eating well, exercising, and limiting alcohol can positively impact fertility chances. Taking medication or supplements can also make a difference.
Legacy’s Male Fertility Supplement contains all of the antioxidants, minerals, and amino acids mentioned above to improve semen quality, including sperm count, motility, morphology, and genetic health.
Find other healthy lifestyle factors to consider in our guide to sperm improvement.
References
- 1. World Health Organization. “WHO laboratory manual for the examination and processing of human semen, 6th ed.,” 2021.
- 2. Van Zyl et al. “Oligozoospermia: recent prognosis and the outcome of 73 pregnancies in oligozoospermic couples,” 2006.
- 3. Karabulut et al. “Male infertility, azoozpermia and cryptozoospermia incidence among three infertility clinics in Turkey,” 2018.
- 4. UNC School of Medicine. “Azoospermia.”
- 5. Sunder et al. “Semen Analysis,” 2022.
- 6. Kumar et al. “Trends of male factor infertility, an important cause of infertility: A review of literature,” 2015.
- 7. Mark et al. “Erectile dysfunction prevalence in the United States: report from the 2021 National Survey of Sexual Wellbeing,” 2024.
- 8. Mazilli et al. “The role of ejaculatory dysfunction on male infertility,” 2020.
- 9. Huijben et al. “Clomiphene citrate for male infertility: A systematic review and meta-analysis,” 2023.
- 10. Hussein et al. “Clomiphene administration for cases of nonobstructive azoospermia: a multicenter study,” 2005.
- 11. Casarini et al. “FSH for the Treatment of Male Infertility,” 2020.
- 12. Fink et al. “Human chorionic gonadotropin treatment: a viable option for management of secondary hypogonadism and male infertility,” 2021.
- 13. Bisht et al. “Oxidative stress and male infertility,” 2017.
- 14. Shoshany et al. “Outcomes of anastrozole in oligozoospermic hypoandrogenic subfertile men,” 2017.
- 15. Peivandi et al. “Effect of letrozole on spermogram parameters and hormonal profile in infertile men: A clinical trial study,” 2019.
- 16. Akmal et al. “Improvement in human semen quality after oral supplementation of vitamin C,” 2006.
- 17. Wang et al. “Effect of vitamin E on Semen Quality Parameters: A Meta-Analysis of a Randomized Controlled Trial,” 2022.
- 18. Zhou et al. “Effects of vitamin E and vitamin C on male infertility: a meta-analysis,” 2002.
- 19. Thakur et al. “Effect of Ubiquinol Therapy on Sperm Parameters and Serum Testosterone Levels in Oligoasthenozoospermic Infertile Men,” 2015.
- 20. Morbat et al. “Effect of Selenium in Treatment of Male Infertility,” 2018.
- 21. Chen et al. “Effectiveness of non-pharmaceutical intervention on sperm quality: a systematic review and network meta-analysis,” 2023.
- 22. Ara et al. “Association of Serum Vitamin D level with Asthenozoospermic Male,” 2024.
- 23. Moghadam et al. “Effects of Vitamin D on Apoptosis and Quality of Sperm in Asthenozoospermia,” 2020.
- 24. Deng et al. “Efficacy and safety of vitamin D in the treatment of idiopathic oligoasthenozoospermia,” 2014.
- 25. Mateus et al. “L-Carnitine and Male Fertility: Is Supplementation Beneficial?,” 2023.
- 26. Irani et al. “The Effect of Folate and Folate Plus Zinc Supplementation on Endocrine Parameters and Sperm Characteristics in Sub-Fertile Men: A Systematic Review and Meta-Analysis,” 2017.




