Table of contents:
- COVID-19 fever
- ACE2 receptors and male fertility
- Short-term impact of COVID-19 on male fertility
- Long-term impact of COVID-19 on male fertility
- Can coronavirus infect the testicles?
- COVID-19 and orchitis
- Can coronavirus be found in semen?
- Can coronavirus be sexually transmitted?
- COVID-19 and pregnancy
- Planning a pregnancy or fertility treatment
- Sperm freezing during COVID-19
- References
UPDATED WITH NEW RESEARCH: NOVEMBER 23, 2020
Each day, we learn more about the novel coronavirus and COVID-19. Here, we speak with some of Legacy’s male fertility experts and examine up-to-date research on COVID-19 and male fertility, pregnancy, and family planning.
For those who are concerned about fertility after COVID-19, any impact on sperm health can be evaluated with sperm testing.
COVID-19 fever and male fertility
One of the primary short-term concerns around COVID-19 and male fertility stems from the known impact of the flu, and its associated fever, on fertility. While COVID-19 is new, “we know quite a lot about viruses, flus, and male infertility,” explains Legacy advisor and reproductive urologist Dr. Paul Turek. “Seasonal flus are known to reduce male fertility… We think that it’s due to the fever associated with the illness, which overheats the testicles.”
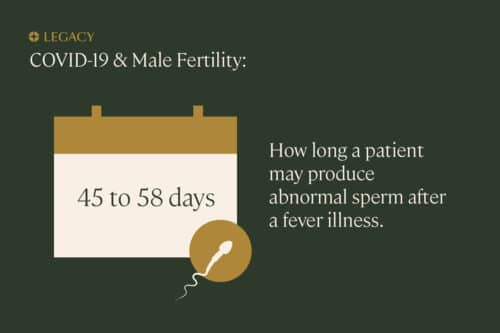
This effect is demonstrated in several case studies of fertile men experiencing fevers. In one, a patient recovering from influenza produced abnormal sperm for 45 days post-fever. In another, sperm count, motility, and genetic health was decreased for over 2 months after the patient’s fever resolved. Considering that one of the primary symptoms of COVID-19 is a high fever, it’s reasonable to assume that men with COVID-19 will also experience reduced fertility.
However, it’s currently believed that the impact of COVID-19 on male fertility will be, like the seasonal flu, temporary. “The effect is similar to that of hot baths or tubs, and is fully reversible,” Dr. Turek explains.
ACE2 receptors in the male reproductive system
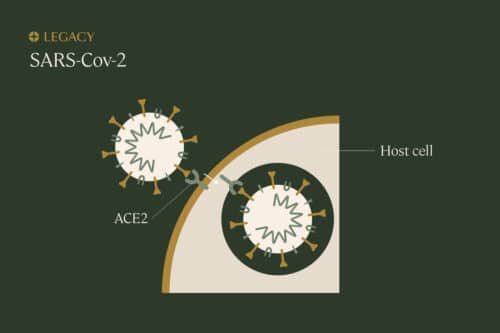
Some researchers have raised concerns around what’s known as ACE2, the protein enzyme to which the novel coronavirus binds; ACE2 provides a sort of “entryway” for the virus to infect cells. ACE2 is on the surface of many cells in the lungs, heart, blood vessels, kidneys, liver, gastrointestinal tract, and reproductive organs. According to researchers, “the testis is one of the organs with high levels of… expression of ACE2,” which means the testes are a probable “target” of the novel coronavirus, and reproductive function could potentially be affected by COVID-19.
COVID-19 does seem to affect male fertility in the short-term
Studies demonstrate COVID-19 may at least have a temporary impact on fertility hormones. Preliminary research revealed that men with novel coronavirus infections had elevated levels of luteinizing hormone (LH) and decreased ratios of testosterone and follicle-stimulating hormone (FSH), compared to healthy men. In another study, nearly 70% of men admitted to a German ICU with COVID-19 had clinically low testosterone levels. In both cases, whether the hormone imbalances were caused by the COVID-19 infection or were a pre-existing factor in the severity of their illness is unknown.
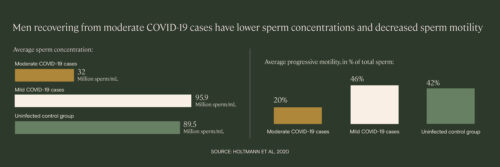
In a small study of men recovering from mild and moderate cases of COVID-19 (Holtmann et al), patients with a moderate case had a “statistically significant impairment of sperm quality” and sperm concentration compared to men without infection, even after up to 54 days post-infection. Two of the moderate cases exhibited azoospermia, a condition in which no sperm at all can be found in the semen sample.
Additionally, brand new (and still unpublished) research from as Israeli medical center reports that patients with moderate COVID-19 symptoms have a 50% reduction in semen volume, sperm concentration, and sperm motility 30 days post-diagnosis.
The long-term impact of COVID-19 on male fertility is less clear
While these studies may indicate that COVID-19 impacts male fertility, there have yet to be any follow-up studies to determine if the effect is reversible (as it is with influenza). As Allan Pacey, PhD, male fertility expert and Legacy advisor, explained, “People who get coronavirus are probably quite unwell. Even influenza will cause a decline in sperm count temporarily… The question is whether it is permanent.”
Holtmann et al, the above-mentioned study of semen parameters in moderate and mild COVID-19 cases, examined men at up to 54 days post-infection, but a follow-up study would be necessary to understand if these changes can be seen long-term. And again, these changes could be due to the fever associated with COVID-19, as opposed to infection of the reproductive system.
And finally, as experts writing in Fertility & Sterility underscore, understanding the impact of COVID-19 on fertility may be confounded by the medications used to treat COVID-19, particularly antivirals and hydroxychloroquine, which are known to be toxic to sperm. For example, in Holtmann et al, three out of the four patients with moderate symptoms of COVID-19 were treated with these medications.
Can the coronavirus infect the testicles?
A recent study points to yes. Researchers collected tissue samples from the testicles of six men who died of COVID-19 and one live patient. Tissue analysis demonstrated that SARS-CoV-2 was found in the testis of one autopsy patient as well as the live patient. This study also found that, in 50% of the patients who had died, spermatogenesis was impaired in direct association with ACE-2 levels.
This study was small, and the disease experienced by the subjects was obviously quite severe. While it doesn’t give us any clear answers about whether COVID-19 has the ability to infiltrate the testis in all cases, it does demonstrate that testicular infection is possible, and lends more support to the idea that fertility is at least temporarily impacted.
COVID-19 and orchitis
There are certain viruses that can cause a painful condition called viral orchitis, inflammation in the testes. While this condition is most closely associated with mumps, SARS—a related infection to COVID-19—has been known to cause orchitis and damage to the testicles.
We have enough information now to conclude that orchitis seems to be a rare, but possible, side effect of COVID-19 infection. While in one study of 253 COVID-19 patients, doctors did not observe any signs of orchitis, in Holtmann et al, one of four patients with a moderate case of COVID-19 experienced testicular discomfort, a symptom of orchitis. Similarly, in a study of 34 male COVID-19 patients, six reported “scrotal discomfort suggestive of viral orchitis.”
At least one diagnosed case of orchitis in a COVID-19 patient has been documented. As doctors note, “spermatocyte function may be compromised secondary to this infection… We characterize the potential complications and importance of fertility follow up.”
While it may take up to a few weeks for the pain of orchitis to subside, there’s a small chance that it will permanently impact male fertility, especially if it only affects one testicle. In cases of mumps, the most common cause of viral orchitis, the condition rarely leads to complete sterility, but may contribute to subfertility; impairment of fertility is estimated to occur in about 13% of patients with unilateral (one-sided) orchitis. The virus typically “has to infect boys at puberty, when the testicles are actively growing, to harm future fertility,” explains Dr. Turek.
Can the novel coronavirus be found in semen?
Conclusions about the presence of the coronavirus in the semen of infected men are conflicting. According to Dr. Pacey, testing semen for viruses has its own set of technical challenges, and more research is currently needed. In Holtmann et al, the coronavirus was not found in the semen of any of the recovered or acutely infected male patients. This finding is consistent with several recent reports in which the coronavirus was not detected in semen.
However, another recent study of 38 men recovering from or infected with COVID-19 concluded that the novel coronavirus was present in the semen samples of 6 subjects. While this may be alarming, it is not necessarily surprising, nor does it indicate a long-term impact of COVID-19 on male fertility. Many viruses have been known to live in the male reproductive tract, even after recovery from the illness they cause.
It’s not currently believed that sperm (or eggs) can carry coronavirus, due to the lack of ACE2 receptors in these cells.
Can COVID-19 be sexually transmitted?
There is currently no evidence to suggest that coronavirus can be transmitted sexually. According to researchers, contact tracing does not indicate that COVID-19 is an STD, and again, conclusions are conflicting as to whether the coronavirus can actually be found in semen (or vaginal fluid). However, the use of condoms would decrease the likelihood of transmission.
COVID-19 and pregnancy
During any pandemic or crisis, we expect essential services like maternity wings and neonatal centers to continue to operate. However, outpatient services at major hospitals and clinics, including their fertility centers, are likely to have their services curtailed or suspended. This time is no different.
Right now, there’s not much data on how COVID-19 might affect pregnant people. We do know that pregnancy alters the immune system in such a way that increases the risk of infections, such as influenza, and could make illness more severe. And we know that related infections such as MERS and SARS can cause adverse pregnancy outcomes, such as miscarriage, premature delivery, intrauterine growth restriction, and maternal death.
Based on this information, American College of Obstetricians and Gynecologists (ACOG) has advised that pregnant women who get COVID-19 may have a higher risk for some complications.
If you already have COVID-19, the Society for Assisted Reproductive Technology (SART) recommends “avoiding getting pregnant for now and waiting until you fully recover before attempting conception (either naturally or via assisted reproductive technology).” Because COVID-19 patients can be asymptomatic, it’s best to get tested to make an informed decision about any potential pregnancies.
Planning a pregnancy or fertility treatment during COVID-19
Reproductive health organizations have advised a cautious approach to conceiving and fertility treatments during the COVID-19 pandemic. As of April 7, the American Society for Reproductive Medicine (ASRM) notes that “if you don’t have COVID-19, there is no medical reason to change your plans regarding trying to conceive. However, there may be logistical, psychological, and emotional reasons to modify your plans… Out of an abundance of caution, you may consider postponing pregnancy.”
Their counterparts abroad, the European Society of Human Reproduction and Embryology (ESHRE) has written that “all fertility patients considering or planning treatment, even if they do not meet the diagnostic criteria for COVID-19 infection, should avoid becoming pregnant at this time.” As of April 23, ESHRE has advocated for recommencing fertility treatments, with caution.
Sperm freezing during the COVID-19 pandemic
Considering data about COVID-19 and male fertility, and the recommendation that couples consider waiting to get pregnant, sperm freezing may be beneficial—both biologically and emotionally—during the coronavirus pandemic.
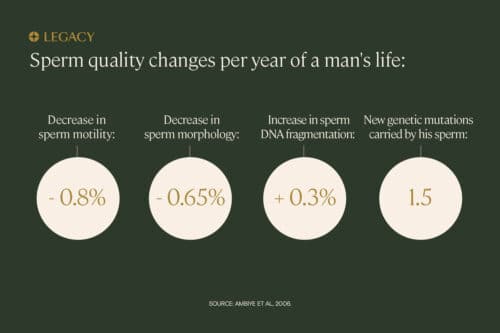
In addition to the potential impact of COVID-19 on fertility (either short-term or long), we also know that time (age) affects sperm quality, especially for men over 35. Sperm acquire a new genetic mutation—which is passed onto offspring—every 8 months. If the COVID-19 pandemic is pushing off your family plans, sperm freezing may be a good option for you.
Social distancing recommendations are still in place, so visiting a doctor’s office or hospital to discuss sperm freezing may not be recommended, or perhaps possible, at the moment. Mail-in sperm testing and freezing options, like the Legacy kit, are a valuable option to preserve your fertility from the safety and comfort of your own home.
Learn more about the Legacy kit.
References:
- D. P. Evenson et al. “Characteristics of human sperm chromatin structure following an episode of influenza and high fever: a case study.” Journal of Andrology, 2000.
- Martin Sergerie et al. “High risk of temporary alteration of semen parameters after recent acute febrile illness.” Fertility & Sterility, 2007.
- Nora Holtmann, MD et al. “Assessment of SARS-CoV-2 in human semen—a cohort study.” Fertility & Sterility, 2020.
- Caibin Fang et al. “ACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-nCoV Infection.” Preprint article, 2020.
- Johnny S. Younis et al. “Is there an impact of the COVID-19 pandemic on male fertility? The ACE2 connection.” American Journal of Physiology—Endocrinology and Metabolism, 2020.
- Saguna Verma et al. “ACE2 receptor expression in testes: implications in coronavirus disease 2019 pathogenesis.” Biology of Reproduction, 2020.
- Ling Ma et al. “Effect of SARS-CoV-2 infection upon male gonadal function: A single center-based study.” Preprint article, 2020.
- Maria Schroeder et al. “The majority of male patients with COVID-19 present low testosterone levels on admission to Intensive Care in Hamburg, Germany: a retrospective cohort study.” Preprint article, 2020.
- Dan Aderka et al. “COVID-19 may harm sperm production.” Unpublished research reported via BioNews, 2020.
- Darshan P. Patel, MD et al. “The jury is still out: COVID-19 and male reproduction.” Fertility & Sterility, 2020.
- Jing Fan et al. “A preliminary study on the reproductive toxicity of GS-5734 on male mice.” Preprint article, 2020.
- Justin K. Achua et al. “Histopathology and Ultrastructural Findings of Fatal COVID-19 Infections on Testis.” World Journal of Men’s Health, 2020.
- Jian Xu et al. “Orchitis: a complication of severe acute respiratory syndrome (SARS).” Biology of Reproduction, 2006.
- Kharbach Youssef et al. “Male genital damage in COVID-19 patients: Are available data relevant?” Asian Journal of Urology, 2020.
- Hassan Alkhatatbeh et al. “Does severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) cause orchitis in patients with coronavirus disease 2019 (COVID-19)?” Arab Journal of Urology, 2020.
- Rachel E. Bridwell, MD et al. “A coronavirus disease 2019 (COVID-19) patient with bilateral orchitis: A case report.” American Journal of Emergency Medicine, 2020.
- M Masarani et al. “Mumps orchitis.” Journal of the Royal Society of Medicine, 2006.
- D. Paoli et al. “Study of SARS-CoV-2 in semen and urine samples of a volunteer with positive naso-pharyngeal swab.” Journal of Endocrinological Investigation, 2020.
- Feng Pan et al. “No evidence of severe acute respiratory syndrome–coronavirus 2 in semen of males recovering from coronavirus disease 2019.” Fertility & Sterility, 2020.
- Ci Song et al. “Absence of 2019 Novel Coronavirus in Semen and Testes of COVID-19 Patients.” Biology of Reproduction, 2020.
- Diangeng Li, PhD et al. “Clinical Characteristics and Results of Semen Tests Among Men With Coronavirus Disease 2019.” JAMA Network Open, 2020.
- Tomer Tur-Kaspa et al. “Is COVID-19 a sexually transmitted disease? A systematic review.” Fertility & Sterility, 2020.
- Guillaume Favre et al. “Guidelines for pregnant women with suspected SARS-CoV-2 infection.” The Lancet—Infectious Diseases, 2020.
- Hákon Jónsson et al. “Parental influence on human germline de novo mutations in 1,548 trios from Iceland.” Nature, 2017.



