Whether to have a vasectomy is a major life decision. Like most big decisions, it comes with a number of considerations — and the opportunity for regret. Although the vast majority of men later feel their vasectomy was the right choice, some have second thoughts. Vasectomy regret is fairly rare, but it’s something to be aware of before undergoing the procedure.
Key takeaways
- The regret rate of vasectomy isn’t very high: between 3 and 10% of men regret their decision and seek a vasectomy reversal.
- Men who are younger when they have a vasectomy are more likely to feel vasectomy regret. Other reasons include a change in relationship status or — rarely — complications from the procedure.
- Thorough pre-op counseling can help prevent vasectomy regret. Freezing sperm before vasectomy can also help by offering a “back-up plan” for those considering vasectomy.
How many men get a vasectomy every year?
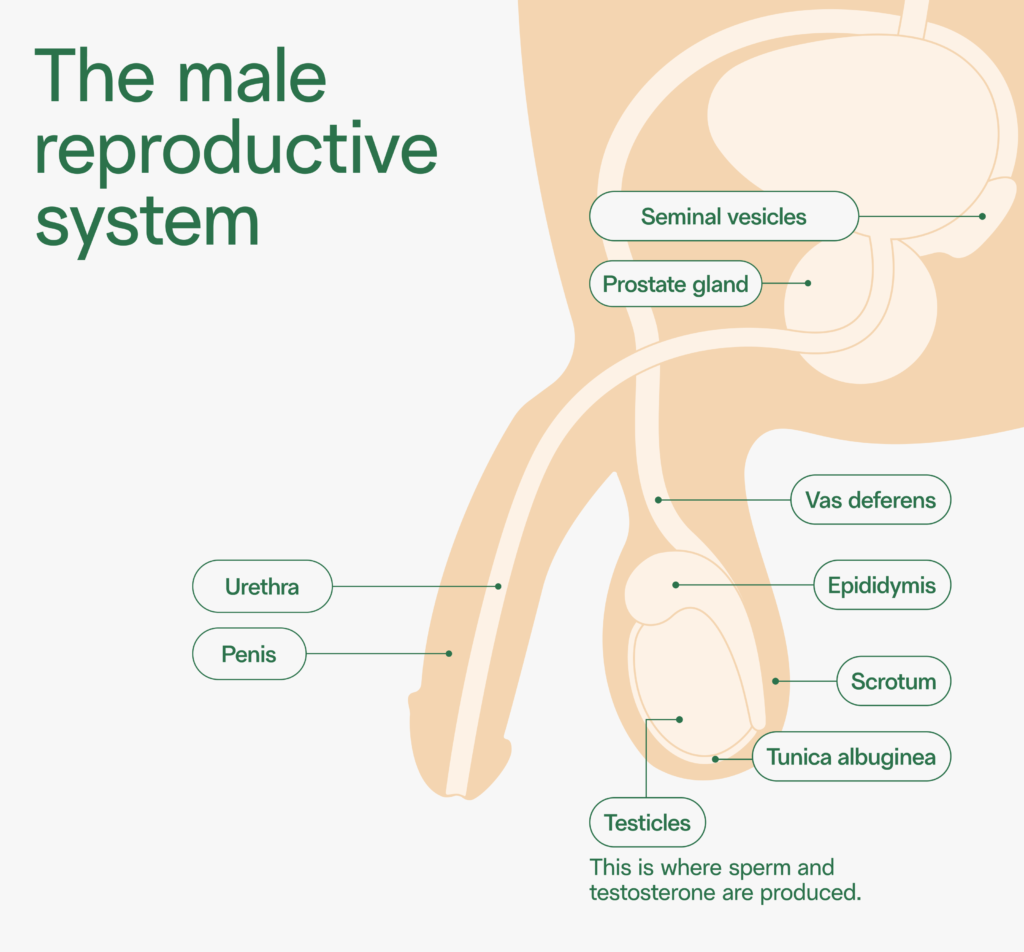
A vasectomy is considered a form of permanent birth control. Vasectomy surgery involves severing the vas deferens, the tube that leads from the testicles — where sperm is produced — to the urethra. This prevents sperm from entering semen and leaving the body.
Learn more about the vasectomy process.
About 500,000 vasectomies are performed each year, and that number is rising, particularly among younger men.1 About 50 million American men have had a vasectomy — that’s approximately 5% of all married men of reproductive age.
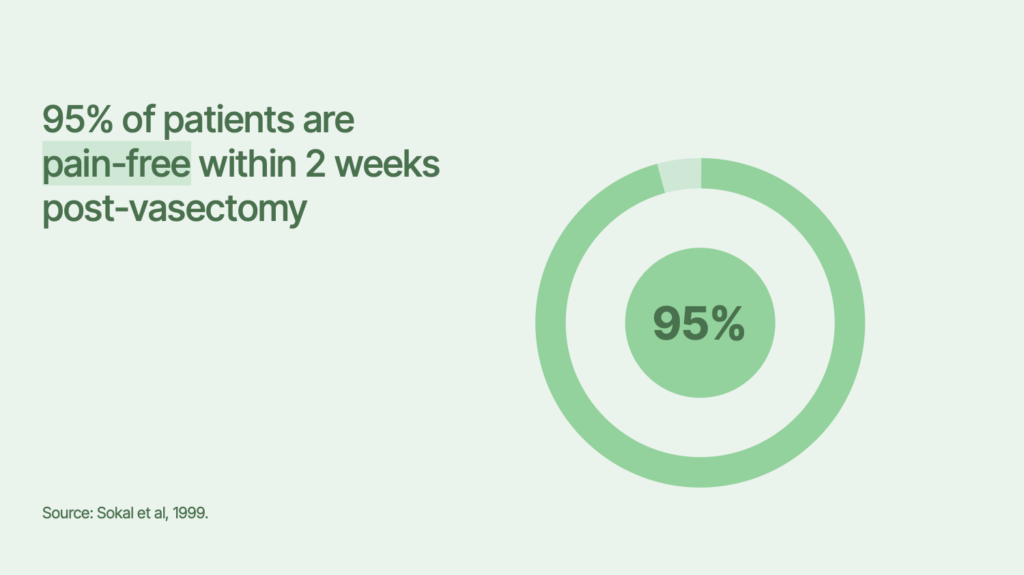
Vasectomy is one of the safest and most effective methods of permanent birth control. Only 1–2% of men who have a vasectomy experience complications, and the procedure is over 99% effective at preventing pregnancy.2
What percentage of men regret getting a vasectomy?
Studies have found that most men are satisfied with their decision to get a vasectomy. But between 3 and 10% of men regret the decision and seek a vasectomy reversal.3
According to a 2022 study published in the journal Health Psychology Research, “the reasons why a patient may regret having a vasectomy tend to center around personal and social factors, such as the age at which they undergo the procedure… or changes in their relationship status.”4
Let’s take a closer look at some of the main factors behind vasectomy regret.
Younger men are more likely to regret their vasectomy
Men who are vasectomized when they’re younger are more likely to have second thoughts. One study found that men who got a vasectomy in their 20s were 12.5 times more inclined to experience vasectomy regret.5
“Some of the regretful men in this age bracket made an impulsive decision to get a vasectomy in a state of emotional turmoil or out of reaction to a stressful situation,” such as a pregnancy scare, a 2022 review of studies found.6
Read more: How old do you have to be to get a vasectomy?
Parental and relationship status can change
Interestingly, that review of research found no boom in vasectomy regret among childless men. Men who are voluntarily childless before their vasectomy are no more likely to regret the procedure than men who had children before getting “the snip.”
Men who’ve lost a child or simply changed their mind about the number of children they want can experience vasectomy regret. A fairly common scenario is that some men may re-evaluate their reproductive plans after getting divorced or starting a new relationship. One study found that 94% of men who regretted their vasectomy had entered a new relationship after the procedure.7
Considering divorce rates are highest between ages 35 and 50 — the ages when men are also most likely to get a vasectomy — it’s important to consider how changes in relationship status might impact vasectomy regret.
Post-vasectomy pain syndrome
A much less common cause of vasectomy regret is post-vasectomy pain syndrome, a condition in which men experience chronic pain in the testicles for three months or more after a vasectomy procedure. It’s estimated that just 1–2% of vasectomy patients experience this.
The causes aren’t well understood. Some research suggests that because sperm can’t leave the vas deferens after a vasectomy, it may accumulate in the testes and epididymis, causing pressure and pain. Discomfort may also be due to damage to the spermatic cord, nerve compression, inflammation, or scar tissue resulting from the procedure.8
Up to 40% of men who have vasectomies will experience a sperm granuloma, which happens when sperm leak out of the cut end of a vas deferens. This can cause inflammation and a benign lump that may be painful, contributing to vasectomy regret. Fortunately, most sperm granulomas resolve on their own after a few months and are most commonly treated with over-the-counter pain relievers.
Do men get depressed after a vasectomy?
The good news is that men who have a vasectomy don’t have a higher likelihood of depression or other mental health concerns, compared to those using other types of birth control.10
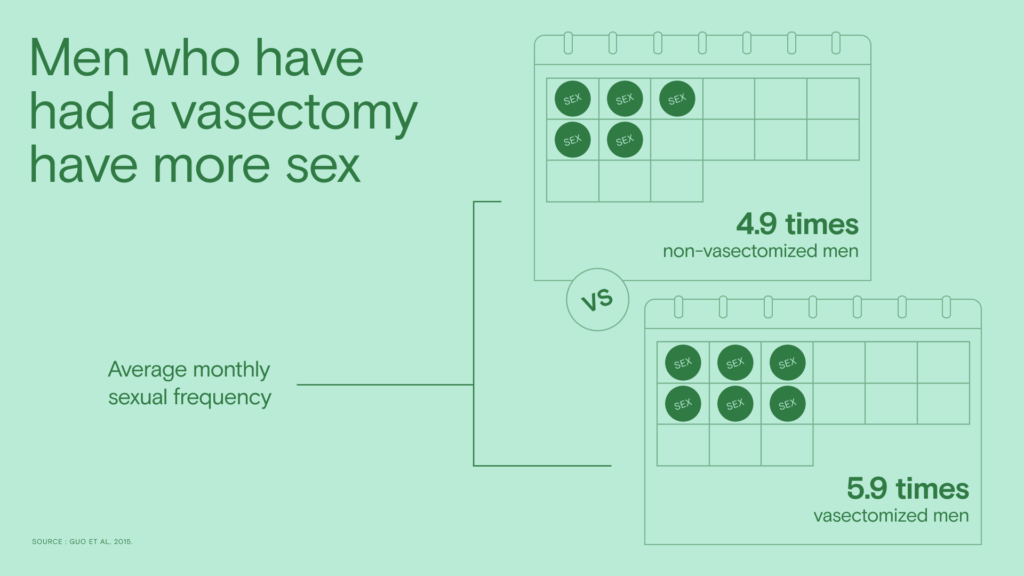
Although it’s rare, men may experience psychological issues after a vasectomy, such as depression, anxiety, or sexual dysfunction. A small number of men might feel “incomplete” after getting a vasectomy, but this is contrary to fact: Having a vasectomy doesn’t reduce your testosterone, make you less “manly” or reduce your sex drive. In fact, most men who have vasectomies report having better sex after the procedure, when anxiety over birth control is alleviated.
Read more: Vasectomy myths & misconceptions
Do men get divorced after a vasectomy?
One study has found that 2.6–10% of couples may experience regret after a vasectomy, which can be related to poor communication or pre-existing relationship issues.10
A 2018 study found that, of 721 men who had a vasectomy, just 49 (6.8%) reported they blamed their relationship breakdown, AKA a breakup or divorce, on their vasectomy procedure.11 A total of 20% had gotten a divorce or broken up with their partner since their vasectomy — but again, that’s not far off from the nationwide divorce rates, which have hovered around 20% for people in their 30s and 40s since 1990.
Options if you’re experiencing vasectomy regret
If you’re saying “I regret my vasectomy” or “my husband had a vasectomy and I regret it,” there are options you can pursue. One of them is a vasectomy reversal, in which a doctor attempts to reconnect the vas deferens. But the procedure isn’t guaranteed; not every vasectomy reversal will be successful at restoring the flow of sperm or enabling pregnancy. In fact, pregnancy rates after vasectomy reversal can be as low as 30%.
Another method of retrieving sperm after a vasectomy is testicular sperm extraction. In this procedure, a doctor pulls sperm from the testicles using a needle or scalpel. (This is also done to extract sperm from non-vasectomized men who have a low sperm concentration, no sperm in their semen, or other conditions that preclude pregnancy.) Studies have found that sperm is successfully retrieved from a TESE procedure 60% of the time.
Preventing vasectomy regret
The most important way to prevent vasectomy regret is to engage in careful and considered decision-making. Thorough counseling from your urologist about the potential side effects and reversibility of your vasectomy is key. Your urologist should also speak to you about the option to freeze your sperm before a vasectomy.
Freezing your sperm is an easy way to reduce the chances of vasectomy regret. If life changes and you decide you’d like to have more biological children, you can utilize your stored sperm samples for intrauterine insemination (IUI) or in vitro fertilization (IVF), and you won’t need to undergo a vasectomy reversal to try for (more) children. Freezing sperm is more affordable and more reliable than vasectomy reversal.
Read more about sperm freezing before a vasectomy.
References
2. Stormont et al, “Vasectomy.” 2024.
3. Anderson et al, “Vasectomy Regret or Lack Thereof.” 2022.
4. Anderson et al, “Vasectomy Regret or Lack Thereof.” 2022.
5. Potts et al, “Patient characteristics associated with vasectomy reversal.” 1999.
6. Anderson et al, “Vasectomy Regret or Lack Thereof.” 2022.
7. Rungby et al, “Vasectomy: Who regrets it and why?” 1994.
8. Sinha et al, “Post-vasectomy pain syndrome: diagnosis, management and treatment options.” 2017.
9. Anderson et al, “Vasectomy Regret or Lack Thereof.” 2022.
10. Shaik et al, “Post-Vasectomy Depression: A Case Report and Literature Review.” 2014.11. Mishriki et al, “Sex, Pain, Relationship Breakdown and Vasectomy.” 2018.



