Vasectomy is a permanent form of male birth control. Vasectomy is performed approximately 500,000 times in the US in any given year, making it a common procedure. Post-vasectomy pain syndrome, on the other hand, is rare — what is it, and why does it happen?
The vasectomy procedure involves sealing off the vas deferens under local anesthesia to prevent sperm from entering the semen. While vasectomy is nearly 99.9% effective at preventing pregnancy, rare complications can arise, such as post-vasectomy pain syndrome, in which patients experience intermittent or constant pain long after the procedure.
Explore the causes of long-term pain after vasectomy, symptoms to look out for, treatments to consider, and other potential causes of testicle pain after vasectomy to rule out other health conditions.
Key takeaways:
- Post-vasectomy pain syndrome affects roughly 1–2% of vasectomy patients.
- Potential causes of pain after vasectomy include damage to testicular structures, nerve compression, inflammation, or scar tissue. Pain may also be caused by non-vasectomy-related problems, such as varicocele and bacterial infections — so a thorough medical examination is important.
- Symptoms of post-vasectomy pain syndrome include a dull ache in one or both testicles, pain with intercourse, and pain with physical exertion.
- Treatments for post-vasectomy pain syndrome include medication, surgical procedures like vasectomy reversal, physical therapy, and acupuncture.
Quick overview: How a vasectomy is performed
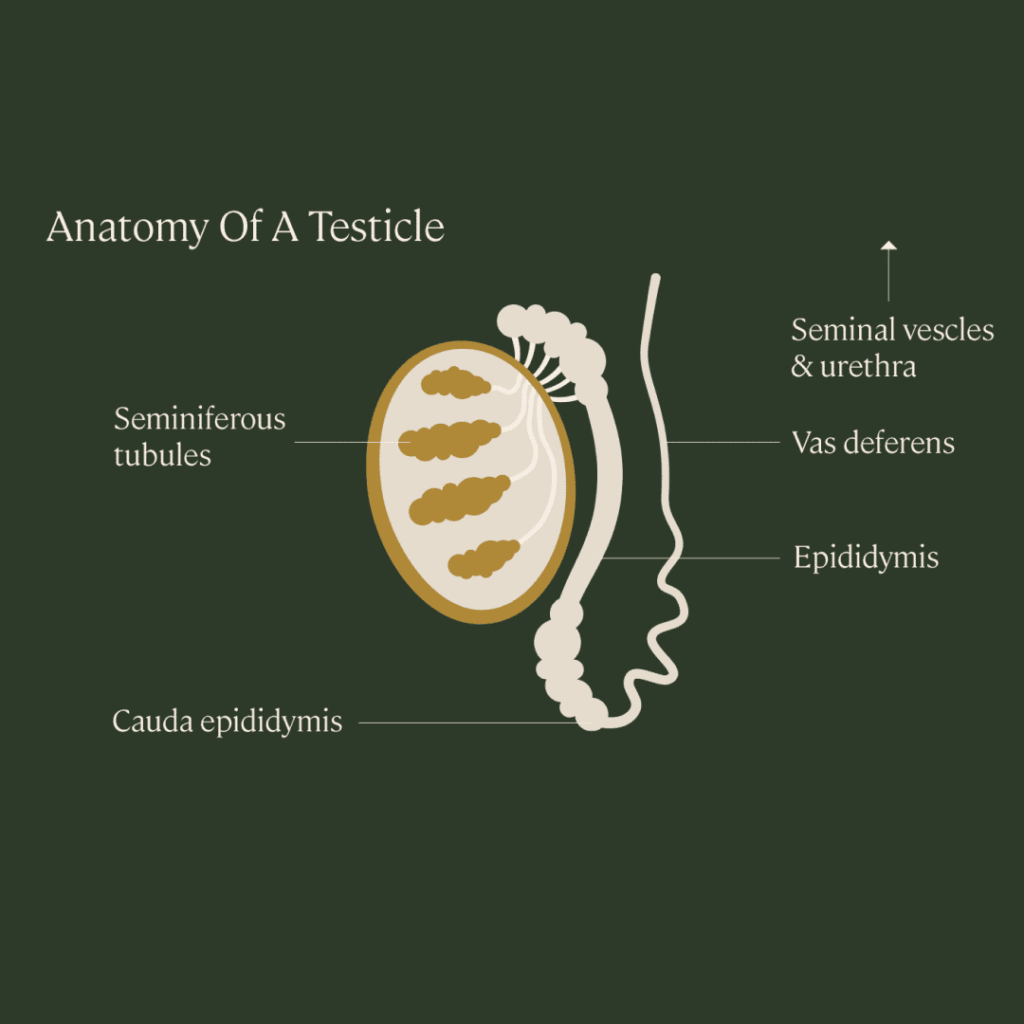
During a vasectomy, a doctor uses tiny tools to make a small opening in the scrotum. Then, they cut or block off the vas deferens, the tubes that transport sperm from the testicles to the urethra in the penis. After the tubes are cut, the patient will still ejaculate, but the semen won’t contain any sperm — the sperm won’t be able to leave the testes or be ejaculated.
What is post-vasectomy pain syndrome?
Vasectomies have a low risk of complications overall. However, there have been reports of a condition called post-vasectomy pain syndrome, in which chronic pain can be felt in one or both testicles for more than three months after the procedure.
Pain can range from an intermittent, dull ache to sharp, constant, and debilitating pain that interferes with one’s quality of life. For some men, the pain is severe enough that they seek treatment, including vasectomy reversal.
How common is post-vasectomy pain syndrome?
Though initial discomfort after vasectomy is common, prolonged pain is not. Post vasectomy pain syndrome affects roughly 1–2% of patients (one study found it was up to 15% of patients, but this is a much higher estimate than most).
Symptoms of post vasectomy pain syndrome
Symptoms may include one or several of the following for longer than three months after surgery:
- A painful or tender scrotum
- A dull ache in one or both testicles
- Pain with intercourse, ejaculation, or both
- Pain with physical exertion
- Discomfort at the site of the vasectomy
- Swelling of the epididymis
- Erectile dysfunction
- Psychological distress
What causes post-vasectomy pain syndrome?
The causes of post vasectomy pain syndrome are not entirely understood. Some studies suggest that, because sperm can’t exit the vas deferens, they may accumulate in the testes and epididymis, increasing pressure and causing pain. Pain has also been attributed to direct damage to spermatic cord structures, compression of nerves in the spermatic cord via inflammation, and scar tissue, as a result of the vasectomy surgery.
A 2013 review of post-vasectomy pain syndrome studies explains that vasectomies that use surgical clips, ties, or cautery to seal the disconnected vas deferens are more likely to lead to an increase in pressure, which can overwhelm the strength of the epididymal or vasal wall. This pain might be felt during ejaculation, or it can be triggered any time the nerves around the vas deferens are agitated.
Otherwise, there are no known risk factors that increase your chances of having post-vasectomy pain syndrome.
Is post-vasectomy pain syndrome “real” or psychological?
While most doctors acknowledge that post-vasectomy pain syndrome is a valid condition, some researchers suggest that vasectomy has the rare potential to cause psychological concerns that affect one’s quality of life more significantly than physiological concerns.
A 2018 study from China found that men with vasectomy for over 15 years did not have extended physiological problems, including no changes to sex hormones and no significant difference in testicular or epididymal size. There was also no increased risk of prostate cancer.
However, researchers did note that some people — especially middle-aged and older men — were influenced at the psychological level after vasectomy. This distress stemmed from fear that the vasectomy would not work and they would have to undergo surgery again, fear of pain, and the view of vasectomy as a “symbolic castration,” representing a loss of masculinity or male identity.
A 2013 review suggests that this psychological impact may contribute to cases of post-vasectomy pain syndrome, stating that “psychogenic causes for the pain must be entertained” when no physiological complications can be found.
Treatments for post vasectomy pain syndrome
Some doctors will prescribe medication such as oral anti-inflammatories, injectable nerve blocks, or antidepressants, depending on the cause of the pain. In some cases, pelvic floor physical therapy or acupuncture can help.
Vasectomy reversal
Vasectomy reversal is the most common and straightforward solution for those who find little success with medical management of post vasectomy pain.
During an outpatient procedure, the tubes (vas deferens) that were cut during a vasectomy are reconnected. Studies show that 84% men with post vasectomy pain syndrome had resolution of pain following vasectomy reversal surgery. In some cases where patients continued to experience pain after reversal, it was attributed to psychological issues. Vasectomy reversal may also reinstate fertility, though success is not guaranteed.
Other surgical treatments for post-vasectomy pain
Some consider an epididymectomy, the surgical removal of the epididymis, the long tube where sperm is transported from the testes to the vas deferens. This procedure has a pain-relief success rate of 50% to 92%, but it eliminates the possibility of a vasectomy reversal down the line.
An orchiectomy, in which one or both testicles are removed, is not always a successful solution either. One study showed that 80% of patients who underwent orchiectomy continued to experience pain.
A micro-denervation of the spermatic cord (MDSC) is a newer surgical option which involves cutting the nerves in the spermatic cord while preserving all the arteries, along with several lymphatic channels. But informed consent is needed as the pain may persist, and in some situations worsen following surgery.
Other possible causes of testicular pain after vasectomy
Not all testicular and abdominal pain after vasectomy is caused by the procedure itself. In some cases, other conditions are at fault, including an enlargement of veins or a bacterial infection.
Varicocele
Also referred to as scrotum varicose veins, a varicocele is an enlargement of the veins within the sac that holds the testicles. Although a varicocele may not produce any symptoms, in some cases it can cause pain that ranges from sharp to dull, which increases with physical exertion.
Infection
For some individuals, an epididymal or testicular infection may develop after a vasectomy, requiring treatment with antibiotics and anti-inflammatory medication. Symptoms of these infections may include discomfort around the genital area, painful urination, and abdominal pain.
Key takeaway: Though post-vasectomy pain syndrome is possible, it is a generally rare occurrence.
If you are considering having a vasectomy, it is recommended to speak to your doctor if you have concerns about developing pain after surgery. Some individuals also choose to freeze their sperm before having a vasectomy to safeguard their fertility and avoid a vasectomy reversal if they change their mind in the future.
Learn more about freezing your sperm in our guide to sperm freezing.