Can getting a vaccine affect fertility, or delay or deter pregnancy? The short answer is no, though there may be temporary side effects to consider. Let’s explore what the research says about how vaccines work and why they are deemed safe for those trying to conceive.
Key takeaways
- Vaccines work to help the body develop immunity to specific diseases by exposing them to small pieces of the virus or bacteria that causes the disease.
- There is no evidence that any vaccines, including COVID-19 vaccines, can cause long-term fertility problems in males or females.
- Fevers associated with vaccines may cause a temporary decline in sperm count or quality.
- Studies indicate that, while some diseases — including COVID-19, mumps, HPV, and hepatitis — may affect fertility, getting vaccinated for the same diseases did not affect fertility at all, and may be protective for fertility.
How vaccines work
Vaccines help the body develop immunity to specific diseases caused by viruses or bacteria. Vaccines typically introduce a small, inactive amount or piece of the “pathogen,” or germ. While this pathogen won’t cause illness, it will trigger the immune system to produce antibodies as if it were actually exposed to the disease.
Afterward, the body is left with a supply of antibodies, T-lymphocytes, and B-lymphocytes (also known as T-cells and B-cells) — immune cells that will be able to fight off that disease if you’re exposed in the future. In this sense, vaccines are like personal trainers for your immune system; they prepare the body for future challenges.
Types of vaccines
The types of vaccines available in the US include live attenuated vaccines, inactivated vaccines, toxoid vaccines, subunit vaccines, mRNA vaccines, and viral vector vaccines. Let’s briefly review how each one works.
Live attenuated vaccines
Live attenuated vaccines contain a weakened version of a living virus or bacteria that can replicate in the body without causing illness.
Examples of live attenuated vaccines:
- Measles, mumps, and rubella (MMR) vaccine
- Varicella (chickenpox) vaccine
- Some seasonal flu vaccines
Inactivated vaccines
Inactivated vaccines use a dead version of the virus or bacteria. Though it can’t replicate, it can still trigger an immune response. Multiple doses may be needed to build up and/or maintain immunity.
Examples of inactivated vaccines:
- Polio vaccine
- Some seasonal flu vaccines
Toxoid vaccines
Some illnesses are caused by toxins produced by bacteria, as opposed to the bacteria itself. A toxoid vaccine introduces an inactive form of that toxin to produce immunity.
Examples of toxoid vaccines:
- Diphtheria vaccine (included in the DTaP or Tdap combination vaccines)
- Tetanus vaccine (included in the DTaP or Tdap combination vaccines)
Subunit vaccines
Subunit vaccines use only specific pieces of a pathogen to trigger an immune response. They’re also called “acellular” vaccines, referring to the fact that they don’t contain a whole cell.
Examples of subunit vaccines:
- Pertussis or “whooping cough” vaccine (included in the DTaP or Tdap combination vaccines)
- Hepatitis B vaccine
mRNA vaccines
Instead of actually containing the pathogen to which they hope to induce immunity, mRNA vaccines contain a type of messenger code that teaches cells to make a subunit of a virus. That piece of the virus then triggers the immune response to create antibodies.
Examples of mRNA vaccines:
- Pfizer-BioNTech and Moderna vaccines for COVID-19, which teach cells to create a controlled amount of the “spike protein” found on the surface of the coronavirus SARS-CoV-2
Viral vector vaccines
Like mRNA vaccines, viral vector vaccines teach cells how to make a particular protein from a virus, triggering the creation of antibodies. In viral vector vaccines, the code is carried inside a modified version of a different virus.
Examples of viral vector vaccines:
- Johnson & Johnson-Janssen and AstraZeneca COVID-19 vaccines, which teach cells to create a controlled amount of the “spike protein” found on the surface of the coronavirus SARS-CoV-2
- Ebola vaccine (still in clinical trials)
Have vaccines ever been shown to affect male fertility?
The short answer: no, vaccines will not impact fertility in the long term.
There is no evidence that any vaccines, including COVID-19 vaccines, cause long-term fertility problems in males or females. And because many infections may affect fertility, getting up-to-date on your vaccines may be an important step in preparing to get pregnant or try to get your partner pregnant.
However, some vaccines may cause a fever. Research suggests that there may be a temporary decline in fertility after a fever — however, research is mixed on whether the short fever associated with vaccination will have a significant effect on sperm count or quality.
Fever and semen parameters
One of the most common side effects associated with vaccines is a low fever, which can occur directly after or up to several days after getting vaccinated. Fever is an expected side effect of vaccination, and indicates that the immune system has kicked into gear and is building its defenses.
However, high body temperatures may negatively affect sperm quality. Sperm are produced most optimally at around 93.2ºF. This is why the testes hang away from the body — to ensure the temperature inside the scrotum is lower than body temp. Fevers can temporarily increase the temperature inside the scrotum.
Research suggests that, depending on the number of hours or days you experience a fever, it may significantly affect your semen parameters (or measures of sperm health). Semen parameters include:
- Sperm concentration: how many sperm are present in the semen
- Motility: what percentage of sperm are moving or “swimming”
- Morphology: what percentage of sperm are the right size, shape, and structure
One small study found that there was a large variation in an individual person’s response to fever. In general, each day of a fever was associated with:
- A 7.1–8.5% decrease in sperm concentration
- A 4.5% decrease in motile sperm
- A 1.6% decrease in morphologically normal sperm
Other studies of fever and male fertility have found this effect is temporary, and semen parameters tend to recover gradually after a fever has resolved. The testes are making sperm constantly, in a process that takes about 72 days. A fever can affect sperm in any stage of development. That means that, after a fever, a person could have altered sperm health for up to 3 months, depending on the severity of the fever.
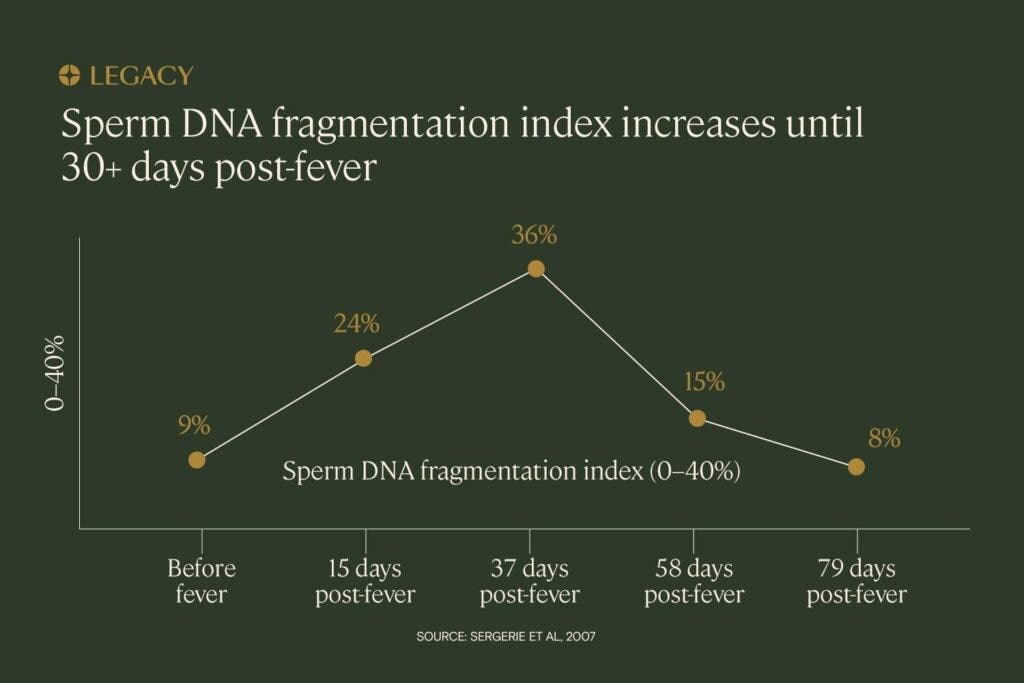
Fever may also affect sperm’s genetic health, or DNA fragmentation. A 2013 study found that a one-day fever associated with influenza had effects on sperm chromatin structure, which resulted in the release of genetically abnormal sperm. At 18 days post-fever, 36% of sperm contained “denatured” or abnormal DNA This percentage decreased gradually as days progressed, again indicating that the effects were temporary.
Will a vaccine-induced fever actually affect male fertility?
It’s also important to note that, in the studies above, the fevers were induced by illnesses, not vaccines. They tended to be higher, around 103°F, while fevers caused by vaccines tend to be lower, less than 102ºF. Vaccine-induced fevers are also likely to be shorter, lasting around 8–16 hours.
Not everyone who gets a vaccine will get a fever. For example, about 16% of people who got the Pfizer COVID-19 vaccine had a fever after the second dose. Some vaccines require more than one dose to be effective, and fevers may be more likely after later doses.
So, while fever after vaccination is a theoretical temporary risk to male fertility, it hasn’t always been shown to affect semen parameters in practice. One study examined the semen parameters of 45 healthy men before and after vaccination with a Pfizer or Moderna mRNA vaccine. Researchers found no decline in sperm count or motility after vaccination.
Long-term effects of vaccines on male fertility?
Clinical trials, follow-up studies, and safety monitoring indicates that no vaccines currently on the market have a long-term impact on semen parameters or male fertility.
In fact, vaccination may be an important step to protecting fertility from illnesses and diseases that can negatively affect sperm health. Several studies have indicated that, while some infections are known to affect fertility, getting vaccinated for those same infections did not affect fertility at all.
HPV vaccine and male fertility
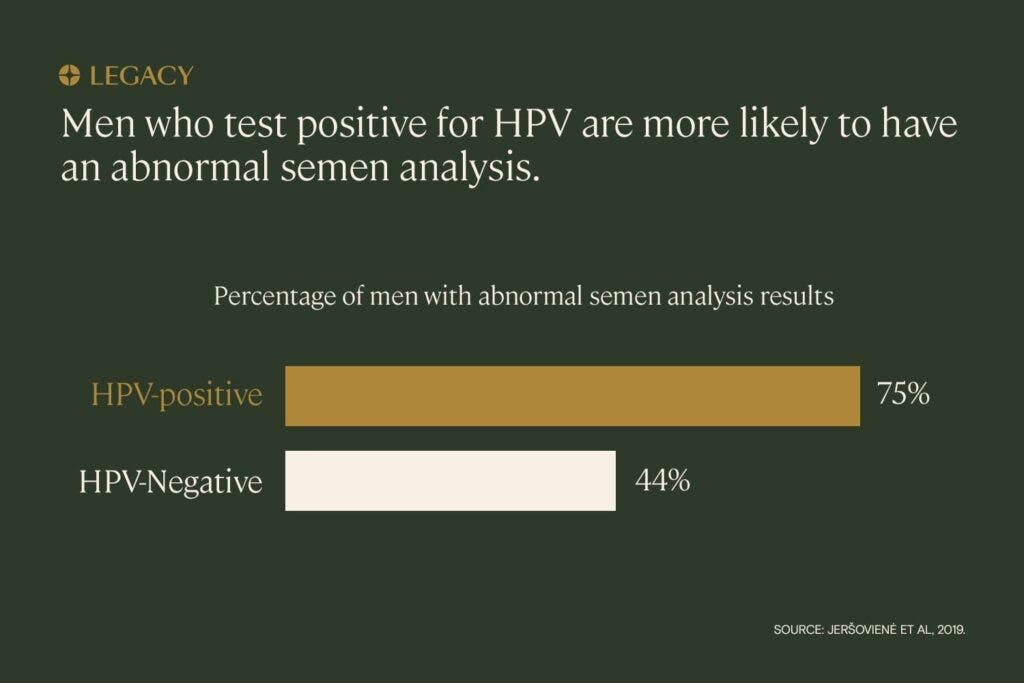
Human papillomavirus (HPV) is associated with infertility in male patients.
A 2010 animal study found that the HPV vaccine has no effects on fertility. After receiving the vaccine, the reproductive markers of male rats, including histomorphology of testes and epididymis, sperm count, and sperm motility, were not impacted.
Interestingly, in one trial, vaccinating men who already had HPV actually improved their fertility — and pregnancy rates were significantly higher in the vaccine group compared to the control group. This is likely because the vaccine triggered action by the immune system to fight the pre-existing infection.
Hepatitis vaccine and male fertility
Similarly, studies show that individuals infected with hepatitis are at higher risk for infertility.
Hepatitis vaccines, on the other hand, are recommended for individuals hoping to conceive a child, and are regularly administered to pregnant people and children to prevent illness and associated fertility issues.
What about the COVID-19 vaccine?
Misinformation about COVID-19 vaccines negatively affecting fertility has persisted throughout the pandemic. A 2021 survey by Kaiser Family Foundation found that almost a third of US respondents had heard that COVID-19 vaccines caused infertility.
Because of myths like these, many pregnant women remain unvaccinated, even though they are at greater risk of experiencing COVID-related complications.
Several studies indicate that COVID-19 vaccines have no long-term effects on male fertility:
In a study of 72 male IVF patients, researchers compared semen parameters before and after receiving two doses of the Pfizer COVID-19 vaccine and found no decrease in sperm count or motility. A study by the University of Miami confirmed similar findings in 45 male participants after 70 days. The length of the second study covers an entire sperm cycle, demonstrating that there are no short-term or long-term effects on sperm parameters.
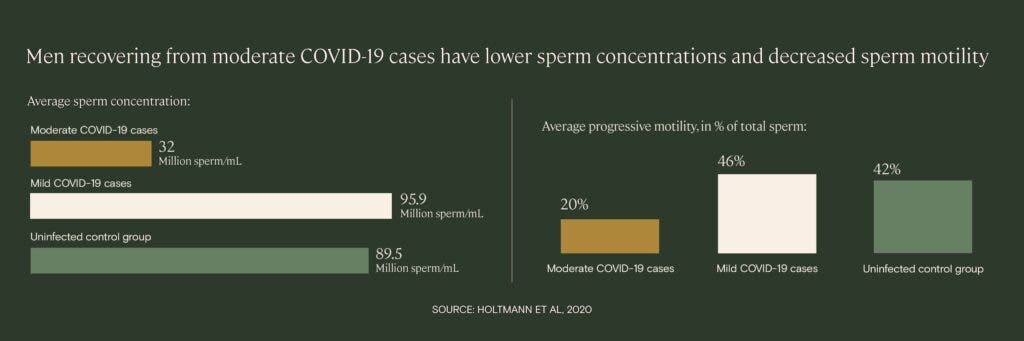
COVID-19 illness is associated with a temporary, but significant, decrease in male fertility. In a small study of men recovering from mild and moderate cases of COVID-19, patients with a moderate case had a “statistically significant impairment of sperm quality” and sperm concentration compared to men without infection, even after up to 54 days post-infection. Two of the moderate cases exhibited azoospermia, a condition in which no sperm at all can be found in the semen sample.
Learn more about COVID-19 and male fertility.
The CDC continues to recommend COVID-19 vaccination for people who are considering conceiving, are pregnant, or are breastfeeding. Similarly, both the Society for Male Reproduction and Urology (SMRU) and the Society for the Study of Male Reproduction (SSMR) recommend that the COVID-19 vaccine should be offered to men desiring fertility.
Should I delay vaccination if I’m trying to conceive?
Bottom line: there’s no reason to put off vaccination if you’re trying to get your partner pregnant. The benefits (of protecting yourself from infection) definitely outweigh the risks.
The one caveat: If you’re doing a cycle of fertility treatment, such as IUI or IVF, you may want to time vaccination so you won’t be providing a semen sample in the period after a possible fever. IVF and IUI are expensive, time-sensitive procedures, and you want to make sure you’re offering your healthiest sperm for optimal chance at success.
Note: This advice is specifically for sperm-producing people. There are different protocols for vaccination before and during pregnancy; if you’re trying to get pregnant, talk to your doctor about the best vaccine schedule for you.
Infectious diseases are real threats to fertility
Just as COVID-19 poses real-life threats to male fertility, so do other infectious diseases, making vaccination a crucial step in protecting one’s chances of having a child.
Mumps orchitis & infertility
Up to 30% of males who get mumps after puberty will experience orchitis, swelling and pain in the testicles. Studies show that just under half of these patients will notice shrinkage of their testicles, and an estimated 1 in 10 will experience a drop in their sperm count.
HPV & infertility
Research has indicated that HPV-infected semen may cause infertility, early miscarriages, and IVF failure. Though the impact of HPV genital tract infection in females is less clear, the presence of the virus in embryos has been associated with reduced pregnancy rate and increased miscarriage rate.
Hepatitis & infertility
Studies show that individuals infected with hepatitis are 1.59 times more likely to experience infertility, mostly due to genetic damage in sperm. HBV-infected patients are also significantly more likely to have varicocele, an enlargement of veins in the scrotum, than their healthy counterparts.
The bottom line: Vaccination is the best way to prevent infection that may affect fertility in the future.
Since so many infectious diseases pose a threat to one’s overall health, including fertility, getting vaccinated is one crucial way to protect your chances of conceiving a child. Find other ways to protect your fertility in our sperm improvement guide, or find out the benefits of freezing your sperm for yet another layer of protection.



