Fertility issues have taken center stage in the 2024 presidential election after vice presidential candidate Tim Walz revealed that his children were conceived with the help of a reproductive procedure known as IUI (intrauterine insemination). Although the discussion of fertility treatments aren’t new to political discourse — in her best-selling memoir, former First Lady Michelle Obama revealed her two daughters were conceived via IVF (in vitro fertilization) — for many people, Walz’s IUI story was the first time they’d heard of the procedure. In the following week, Google searches for IUI vs. IVF more than tripled.
Although both IUI and IVF are forms of assisted reproduction utilized to achieve pregnancy, they differ in complexity and may be used to address different types of infertility. Here are the key differences between IUI vs. IVF.
Key takeaways
- IUI and IVF are forms of assisted reproduction, methods of medical assistance for getting or staying pregnant.
- During IUI, washed and prepared sperm are inserted directly into the uterus at the time of ovulation.
- In an IVF cycle, eggs are surgically removed from the body and combined with sperm to create embryos, which can then be placed back into the uterus in the hope of achieving pregnancy.
- Other differences between IUI vs. IVF include cost, price, and success rates.
What is IUI?
Intrauterine insemination (IUI) is a non-surgical procedure in which sperm are washed and inserted directly into the uterus during ovulation. By reducing the obstacles to fertilization, IUI can improve the chances of pregnancy.
IUI may be performed:
- In cases of female-factor infertility, such as polycystic ovarian syndrome (PCOS) or other ovary conditions, often alongside medication that promotes ovulation
- In cases of mild male-factor infertility
- In cases of endometriosis, a condition when uterine tissue grows outside the uterus)
- When the condition of the cervix or ovaries makes it difficult to conceive
- When a female partner is allergic to semen or produces antisperm antibodies
- To create a pregnancy with donor or frozen sperm
How IUI is performed
IUI is performed at the time of ovulation. Ovulation can be tracked using bloodwork for specific hormones and/or ultrasound. Some people who plan to do an IUI will take prescription medication to help stimulate or properly time ovulation.
The IUI procedure starts with a semen sample, which can be fresh or frozen. A laboratory scientist will process the sample with a technique called sperm washing, in which the proteins and contaminants of the semen are removed to isolate healthy sperm.
During the IUI, a healthcare provider inserts the washed sperm directly into the uterus with a catheter. This takes about 10 minutes. In a successful IUI procedure, the sperm will fertilize the egg to create an embryo. If the embryo develops properly and implants in the uterine lining, the treatment has achieved pregnancy.
Why choose IUI vs. IVF?
IUI is more affordable and less invasive than IVF, since it doesn’t involve surgery and can often be completed with oral medications, instead of injectable hormones. IUI can also be performed by an OB/GYN or midwife, whereas IVF can only be managed by a reproductive endocrinology team with an embryology lab.
IUI is often performed as the first treatment for infertility, including unexplained infertility. IUI can help achieve pregnancy in cases of mild to moderate forms of male infertility, including sperm quality issues like lower motility (movement).
In more severe cases of male infertility, IVF (in vitro fertilization) may be recommended. If a woman is over the age of 40, a doctor may recommend going straight to IVF.
What is IVF?
In vitro fertilization (IVF) is a form of assisted reproduction in which eggs are combined with sperm outside the body. It’s more invasive and expensive than IUI, but it also has a higher success rate.
The female patient takes medication that stimulates the ovaries to produce multiple eggs. The fertility doctor will surgically remove the eggs from the ovaries and an embryologist will combine them with sperm in a laboratory to create one or more embryos.
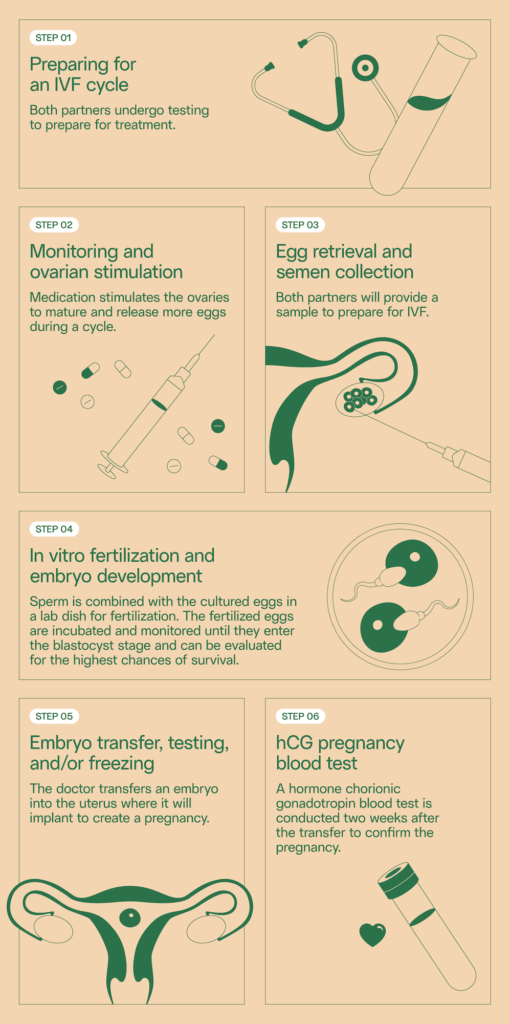
How IVF is performed
An IVF cycle takes about two to three weeks. The female patient injects fertility medications daily, stimulating the ovaries to produce multiple mature eggs. A healthcare provider then removes the eggs from the ovaries in a surgical procedure called an egg retrieval. The retrieval involves a needle puncture through the vaginal wall and into the ovaries to collect the eggs. It’s performed under anesthesia.
The retrieved eggs are combined with sperm in a lab to enable fertilization. Fertilized eggs hopefully develop into blastocysts (AKA zygotes), which can be frozen, genetically tested, and/or transferred to a uterus three to six days after fertilization.
Two weeks after embryo transfer, a pregnancy test can indicate whether the procedure was successful.
Why choose IVF vs. IUI?
IVF is often used by people with:
- Blocked fallopian tubes or differing anatomy of the cervix
- Poor egg quality or low ovarian reserve, often experienced with age
- Endometriosis
- Sperm quality issues, such as low concentration or motility
In cases of severe male-factor infertility, IVF may be paired with intracytoplasmic sperm injection (ICSI), in which a single sperm is injected directly into each mature egg. ICSI can enable pregnancy even in cases of very low sperm concentration or motility.
ICSI may also be used when a patient is working with limited numbers of frozen sperm. For example, if a cancer patient froze sperm before losing their testicles to orchiectomy, their doctor might recommend IVF with ICSI to maximize the number of fertilized embryos they’re able to create with that sperm.
IVF is also used to prevent miscarriage or the conveyance of genetic disorders to offspring. Embryos can undergo screening, known as preimplantation genetic testing, before being transferred to the uterus for pregnancy. This testing can ensure that the medical team only transfer embryos with the proper number of chromosomes, reducing the chances for pregnancy loss, or embryos without specific genetic mutations, such as the mutation that causes cystic fibrosis.
Lastly, IVF may be chosen when earlier IUI cycles weren’t successful. Typically, patients will try 3–6 IUI treatments before trying IVF, unless specific conditions push their doctor to recommend IVF right away.
IUI vs. IVF success rates
Both IUI and IVF can increase the chances of pregnancy, but their success rates differ. It’s important to know that many factors can affect success rates, including both partners’ ages and — specific to IVF — the quality and number of embryos that are transferred.
IUI success rates average about 10–20% per cycle. This varies by age. One analysis of over 4,000 IUI cycles found average IUI pregnancy rates by age.1
| Age of female patient | Chance of pregnancy per IUI |
| 24 and under | 20% |
| 25–29 | 13% |
| 30–34 | 11% |
| 35–41 | 9% |
| 42–43 | 6% |
| 43 and over | 3% |
These numbers may seem low. But for perspective: the chance of getting pregnant through sex is about 20% each month. (This also declines with age.)
The success rate of IVF also varies by age. According to the CDC’s database, IVF success rates can be anywhere from 8–50% depending on the age of the female patient.2
| Age of female patient | Chance of pregnancy per egg retrieval |
| 35 and under | 51% |
| 35–37 | 36% |
| 38–40 | 23% |
| 40 and over | 8% |
As you can see, IVF success rates are higher on average, but still decrease with age.
Paternal age also impacts success rates with both IUI and IVF, although slightly less dramatically. One analysis of over 17,000 IUI cycles found that success rates were highest when the biological father was under 40.3
When it comes to IVF, men over 35 have significantly lower success rates, according to a study from 2023.4
| Age of male patient | Chance of pregnancy per embryo transfer |
| Under 35 | 31% |
| 35–39 | 22% |
| 40 and over | 20% |
Learn more about male fertility decline with age.
IUI vs. IVF success rates with frozen sperm
Both IUI and IVF can be performed using frozen sperm. Multiple studies have found that there is little difference in success rates when using frozen sperm, compared to “fresh” never-frozen sperm.
When you consider the decline in male fertility with age, it becomes clear that sperm freezing is a great insurance policy for those who may want children later in life.
IUI vs IVF cost
The price of IUI is significantly less than IVF. The cost of an IUI procedure can range from $300 to $4,000 without insurance, depending on the fertility clinic, medication costs, necessary tests, and follow-up.
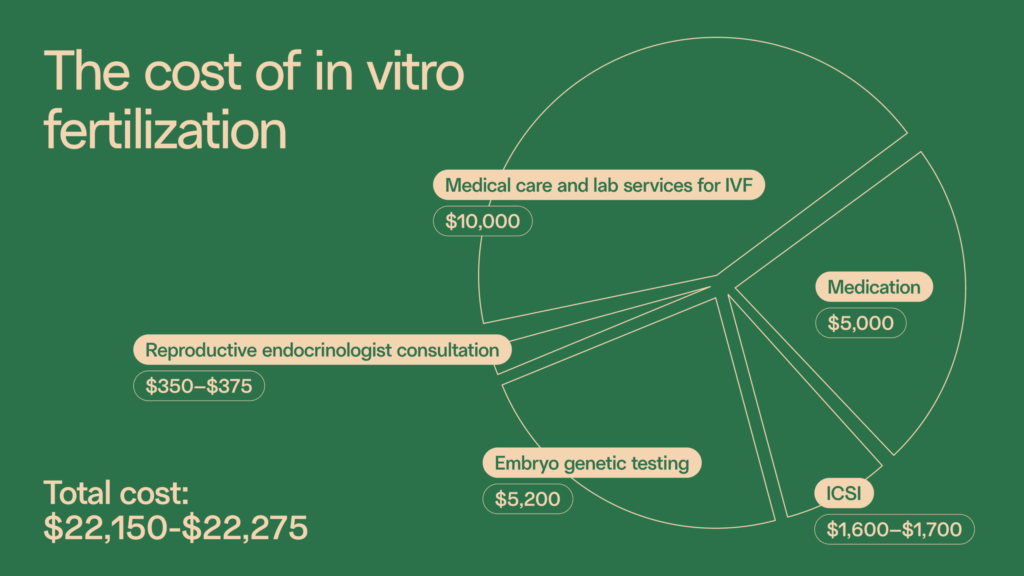
The average cost of an IVF cycle is about $15,000, plus about $5,000 for medication, without insurance.
Because IUI is less effective than IVF, couples may need several cycles of IUI, which can bring the overall price of IUI to about 50% of IVF.
Semen analysis before IUI or IVF
Not sure if IUI or IVF is right for you?
A semen analysis empowers you with the data you need to make informed decisions about your next steps. Legacy’s at-home semen analysis reports on every industry standard measure of sperm health. including sperm concentration (or count), motility, and morphology (shape).
Our advanced semen analysis measures DNA fragmentation, which measures what percentage of sperm in a sample has DNA damage, a factor that can impact IUI and IVF success rates.
Get started with sperm testing.
References
- 1. Schorsch et al, “Success Rate of Inseminations Dependent on Maternal Age? An Analysis of 4246 Insemination Cycles.” 2013.
- 2. Center for Disease Control, “Assisted Reproductive Technology (ART) Data.” 2021.
- 3. Belloc et al, “Effect of maternal and paternal age on pregnancy and miscarriage rates after intrauterine insemination.” 2008.
- 4. Lu et al, “Effect of advanced paternal age on reproductive outcomes in IVF cycles of non-male-factor infertility: a retrospective cohort study.” 2023.



