Previously, a lot of focus has been placed on maternal age when analyzing the success of artificial reproductive technology (ART). But what about paternal age and fertility?
The American College of Obstetricians and Gynecologists (ACOG) states that after people with ovaries reach age 30, their fertility declines. Once they reach the mid-30s, this decline gets even more rapid. The reduction in fertility through maternal age is believed to impact the success of ARTs such as IVF and IUI and the outcome of pregnancy.
However, a recent study published in the journal Human Reproduction focuses on paternal age. It highlights that paternal age could impact ART success and live birth rates more than previously thought. Let’s review the study, and what it might mean for you.
Key takeaways
- A new study of 18,825 IVF cycles found that the age of the male partner correlated with success rates.
- This study adds to the bank of evidence supporting the idea that male fertility decreases with age.
- Men should consider freezing their sperm at a younger age, especially if they may, or plan to, have kids later in life.
Studying the impact of paternal age on fertility
First, let’s look at the study in a little more detail. Over a period of two years, the scientists analyzed nearly 19,000 IVF cycles from the UK’s national, anonymized registry. The research team conducted a retrospective analysis, which means they looked backward at data collected from previous patients.
The couples in the study underwent IVF with a fresh, single embryo transfer, due to unexplained or tubal infertility. The trial excluded people doing IVF due to male-factor infertility, donor sperm, or preimplantation genetic testing.
The study found that, overall, the fertility of a couple declined with the age of the male partner.
| Age of male partner | Live birth rate per embryo transfer |
| ≤ 39 years old | 39.1% |
| 40–44 years old | 25.9% |
| 45–50 years old | 23.0% |
| 51–55 years old | 22.9% |
The study also found that male and female partner age have a compounding effect on fertility. The most significant result from the study was in women aged 35–40. There was a substantial drop in the live birth rate for this age group if the male partner was 40 and above. Interestingly, if the woman was under 35 or over 40, the paternal age made a negligible difference to live birth rates.
The study highlights that paternal age has an impact on IVF success for many couples. Maternal age has always been a primary consideration with regard to the success of ART, but fertility is very much a male issue too. This research demonstrates that paternal age should be considered when discussing fertility treatments and chances of success with couples. Additionally, men should be aware that their fertility, too, declines significantly with age.
What previous research says about age and male fertility
The study discussed above ties into a growing body of research highlighting the impact of paternal age on fertility. The Centers for Disease Control and Prevention (CDC) reports fertility declines in most men after age 40.
Previous studies have shown conception is 30% less likely for men over the age of 40, compared to men younger than 30. Sperm parameters such as concentration, motility, and morphology are seen to decline after 40.
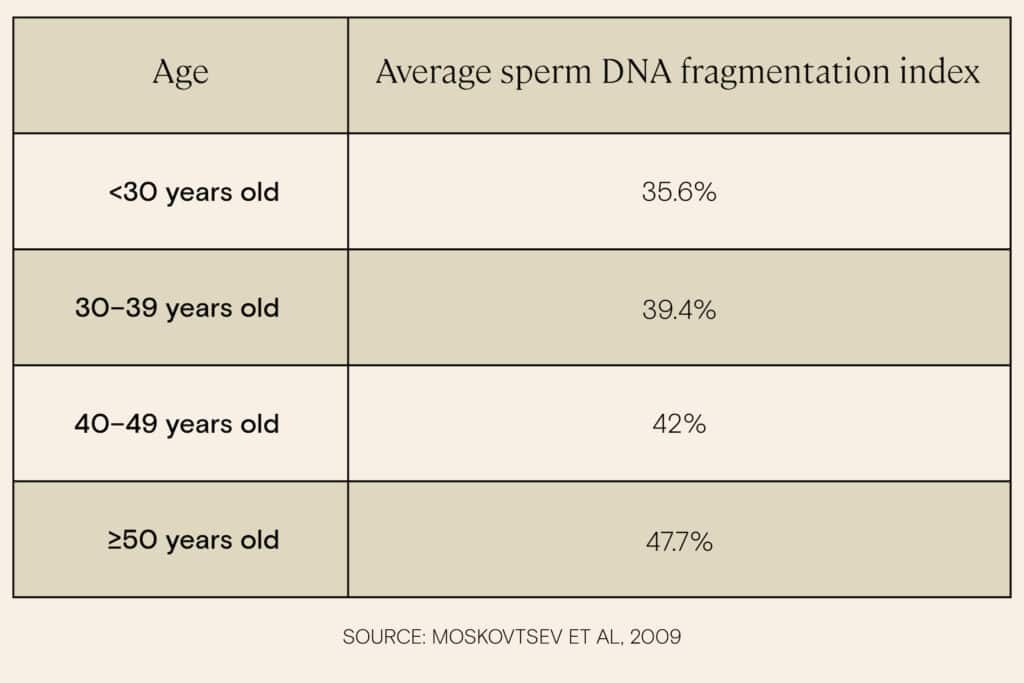
Additionally, studies find that sperm DNA fragmentation — the level of damage to the genetic material inside sperm — measures increase measurably with age.
And it isn’t just a concern about getting pregnant. Men over the age of 45 see an increased risk of birthing complications and adverse birth outcomes.
Essentially, most of the research points to an age-related decrease in male fertility after 35, with the decline progressing from there.
What this means for you
This study adds evidence to the fact that sperm-producing people have a biological clock, too.
If you’re planning to have kids later in life, freeze your sperm. Sperm freezing preserves the quality of your sperm, enabling you to have younger, healthier sperm to work with if you’re trying to have kids later in life.
Who should freeze their sperm?
Consider freezing your sperm if:
- You don’t want kids right now, but you may want them when you are older. Or you’re not sure if you want kids or not in the future.
- You need to use fertility treatments like IUI or IVF to conceive.
- You’re considering a vasectomy.
- You are going to start gender-affirming hormone therapy.
- You need to have a medical treatment that may affect fertility, such as chemotherapy.
- You have a profession that may put your fertility at risk, such as serving in the military.
How sperm freezing works
Before freezing sperm, it’s advised to have a semen analysis to check your sperm parameters and ensure you are freezing healthy sperm. You will also need to screen for sexually transmitted infections — especially if you are undergoing IVF.
To freeze your sperm, you’ll have to supply a sample through masturbation. You can do this in a private room at a fertility clinic, or via an at-home sperm freezing and testing service (like Legacy’s) that allows you to provide your sample in the comfort of your home.
Sperm is frozen and stored at the temperature of -196ºC, where all biological activity pauses, in a special storage facility. The freezing process does not significantly affect the quality of your sperm. Once frozen, you can store sperm indefinitely.
Cost of sperm freezing
In most conventional clinics, The total sperm analysis and storage cost can reach up to $1,000. You then may have to pay ongoing sperm storage costs of around $300–500 (or more) per year.
If you are looking for more transparent and flexible options, then Legacy offers several choices for testing and freezing your sperm, with annual, 5-year, and lifetime storage options. These are a fraction of traditional sperm freezing costs.
See the range of Legacy sperm testing & freezing options.



