Sexually transmitted infections or diseases, including chlamydia, gonorrhea, herpes, and HIV. may have a short-term or even long-term impact on sperm health and male fertility. Let’s unpack how STIs can affect male fertility, plus how to protect your fertility and what to do if you test positive for an STI. Proactive STD testing, or STD testing kits are always a good option.
Key takeaways
- STIs can affect male fertility or, in some cases, even cause infertility. Gonorrhea, chlamydia, herpes, HIV, HPV, and mycoplasma/ureaplasma may all affect fertility or family-building plans.
- If left undetected or untreated, STIs can spread to a female partner, potentially affecting female fertility or pregnancy.
- The best way to protect your fertility is to use barrier protection (if you’re not trying to conceive), test regularly, and treat any infections promptly.
What is an STI?
A sexually transmitted infection is an illness that’s primarily or most commonly spread by sexual contract. The pathogen, or germ (such a bacteria, virus, or parasite), that cause sexually transmitted infections may pass from person-to-person via blood, semen or vaginal fluid, or skin-to-skin contact in the genital region.
What’s the difference between an STI and an STD? An STI, or sexually transmitted infection, is the presence of any of the pathogens, even if a person doesn’t develop symptoms. An STD, or sexually transmitted disease, is the actual illness caused by those pathogens. We’re using STI here because these pathogens can impact fertility even if they never cause symptoms of disease.
Can STIs cause male-factor infertility?
The short answer is yes, certain STIs/STDs can cause male fertility issues, especially if left untreated. STIs are more likely to affect female fertility than male fertility, because people with penises are more likely to have identifiable STI symptoms and therefore receive early treatment.
However, STIs can affect male-factor infertility whether you show symptoms or not.
STIs that can impact male fertility
Most sexually transmitted infections can have a short-term adverse effect on male fertility, until the infection is cleared. Some infections are long-term or chronic, or can have a more significant effect on male fertility. Here, we’ll discuss chlamydia, gonorrhea, herpes, HIV, HPV, and mycoplasma/ureaplasma and how they can impact male fertility.
Chlamydia
For people with penises, symptoms of chlamydia include chlamydia will experience pain in their genitals or discharge, but many people will have no symptoms, making regular STD testing and STD screening important.
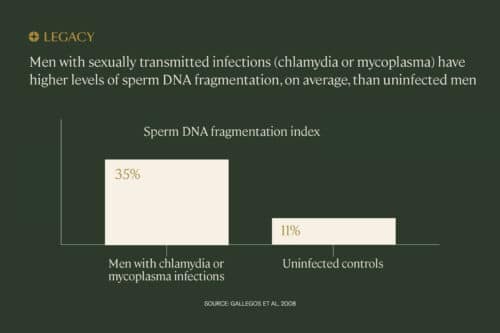
Chlamydia can affect male fertility. In one study, sperm DNA fragmentation in chlamydia-positive men was 3.2 times higher than in healthy patients. Sperm DNA fragmentation is damage to the genetic material carried by sperm, which can contribute to male-factor infertility.
Because chlamydia is a bacterial infection, it can be cleared with antibiotics. In the study mentioned above, antibiotics helped reverse the fragmentation, but catching it early gave the best results.
Those who leave chlamydia untreated are also more likely to transmit the infection to a female partner, where it may not be detected as easily. For people with vaginas, chlamydia doesn’t cause fertility issues if it’s treated promptly. But the longer it goes untreated, the more likely a person is to develop pelvic inflammatory disease (PID), an infection of one or more of the upper reproductive organs.
People with PID are at risk of developing scarring in their fallopian tubes, which could lead to infertility. Studies demonstrate that approximately 21% of women who have had one or more episodes of PID experience infertility. As such, proactive STD screening is an important step.
Gonorrhea
Gonorrhea is another bacterial infection. Some people with gonorrhea will experience pain while urinating or discharge, but many will have no symptoms. Gonorrhea may not develop symptoms for up to 30 days, making it more likely that partners will transmit the infection to each other before seeking treatment. Untreated gonorrhea, like chlamydia, can cause PID in people with uteruses, making it harder to conceive later.
With regard to male fertility, studies show a connection between gonorrhea and the development of urethritis, inflammation of the urethra. Urethritis can also lead to epididymo-orchitis. Orchitis is an inflammation of the testicles, often accompanied by an inflammation of the coiled tube at the back of the testicle that carries sperm (the epididymis).
These inflammatory conditions can affect male fertility, and it could be long-term. In one small study, 60% of men who developed urethritis and epididymo-orchitis due to gonorrhea had abnormal semen parameters two years post-infection.
Herpes
Herpes is a family of viruses that causes sores that can be painful or itchy. Herpes simplex virus (HSV)-1 most commonly causes oral herpes, also known as “cold sores,” while HSV-2 most commonly causes genital herpes. Both HSV-1 and 2 can be sexually transmitted.
Herpes may be one of the most common sexually transmitted infections, but surprisingly few studies have been completed to explore its connection to male-factor infertility. In one small-scale study of 70 men, researchers found a potential connection between a herpes diagnosis and lowered sperm count. The connection was found with both HSV-1 and 2.
As a virus, herpes can’t be cleared up with antibiotics like some other STIs. However, antiviral drugs can help manage the infection, reduce breakouts, and decrease someone’s likelihood of spreading herpes. It’s unknown if the use of antiviral drugs can affect male fertility for people with herpes.
Most important is actually the herpes status of the birthing parent. While herpes is a relatively harmless infection for a healthy adult, it can be serious or even fatal for a newborn who contracts it during vaginal delivery.
HIV
HIV (human immunodeficiency virus) is a virus that attacks the immune system, and can be transmitted through sex or other activities in which blood, semen, or vaginal fluids are exchanged. Some people with HIV will have temporary flu-like symptoms, while others will have no symptoms. Regular STD testing is the best way to detect and prevent the spread of HIV.
HIV can cause the life-threatening illness AIDS (acquired immunodeficiency syndrome) if it’s not treated, and is able to significantly damage the immune system. But the long-term effects of HIV have changed dramatically since the disease was first discovered. Patients have much longer life expectancies and are able to lead normal, relatively healthy lives with the help of antiretroviral therapy and preventative medications.
AIDS is associated with poor semen parameters. In minimally symptomatic or asymptomatic people with HIV, male fertility does not seem to be impacted by the virus. However, the antiretroviral therapy used to manage HIV may have the unintended effect of impacting male fertility. Researchers have found that men with medication-managed HIV have reduced sperm motility, lower sperm counts, and lower semen volume compared to healthy men.
One of the biggest fertility concerns with an HIV diagnosis is family planning safety. In a couple where only one partner is HIV-positive, attempting natural conception carries a risk of transmission to the uninfected partner (even if that risk is small, thanks to medication like PrEP).
HIV-positive people with sperm may explore fertility options that do not involve natural conception. Semen washing, for example, is a technique in which sperm is removed from the seminal fluid for use in insemination (IUI) or IVF, and may be a very effective preventative measure for HIV transmission. One study looked at over 11,000 cycles of IVF/IUI that used washed semen samples from male HIV patients, and found not a single instance of transmission to the female partner.
HPV
Human papillomavirus or HPV is the virus that causes genital warts. HPV is the most common STI there is, and quite a bit of evidence suggests that it affects fertility parameters for both sexes. In people with uteruses, HPV may be a risk factor for infertility and poor pregnancy outcomes (though it may not be an independent cause of infertility).
HPV may also affect male fertility. In a 2019 study, researchers studied semen samples from 20 male patients who were HPV positive. They found that HPV infection was detected more frequently among men with abnormal sperm parameters, suggesting that HPV may have an impact on sperm production — 75% of men who tested positive for HPV had abnormal semen analysis results, compared to 44% of men who tested negative for HPV.
Mycoplasma/ureaplasma
Mycoplasma is a bacteria that can infect many bodily organs. Ureaplasma is one type of mycoplasma bacteria that commonly affects the genitals and urinary tract. (These are considered sexually transmitted infections, but they can spread or develop in other ways as well.) Symptoms of ureaplasma infection include pain during urination, belly pain, and urethra swelling or discharge.
Studies point to a link between these bacteria and male fertility issues. In one literature review, researchers found that infection with certain strains (U. urealyticum and M. hominis) was significantly more prevalent among those with male-factor infertility. However, other strains did not have any correlation to male fertility.
Like chlamydia, mycoplasma infection has been associated with increased DNA fragmentation in sperm. Although antibiotics do seem to reduce or reverse the effects, we still don’t fully understand the links between these bacterium and sperm quality or overall male fertility.
How STIs can indirectly affect male fertility
Sometimes, it’s not the STI itself that causes male-factor infertility issues. Some STIs can cause secondary issues that could then affect male fertility. STD screening can help uncover some of these indirect effects.
Chlamydia and gonorrhea both have the potential to cause urethritis, inflammation of the urethra, the tube that carries urine from the bladder and semen from the testicles. Certain mycoplasma and ureaplasma organisms can also cause urethritis.
In people with vaginas, this condition can sometimes lead to pelvic inflammatory disease, thanks to infections traveling through the lower reproductive system.
As mentioned above, for people with penises, urethritis or untreated STIs can lead to epididymo-orchitis. Orchitis is an inflammation of the testes. Bacterial epididymo-orchitis often results from untreated chlamydia or gonorrhea infection.
As previously mentioned, research suggests that urethritis and epididymo-orchitis may have a long-term effect on male fertility, impairing semen parameters for several years. The best way to prevent urethritis and epididymo-orchitis is regular STI testing and prompt treatment of STIs.
Protecting male fertility from STIs
- Use a barrier method. Birth control pills and spermicide are great for family planning, but don’t protect against STIs. For that, you’ll need a barrier method such as a condom.
- Consider regular testing. STD screening is part of a responsible approach to your reproductive health. The CDC recommends STD testing at least once a year, but potentially every 3–6 months if you have multiple partners.
Legacy offers an easy at-home STI testing kit that can accurately detect 6 common STIs that may affect male fertility. An at-home STI testing kit is one of the most convenient ways to safeguard your fertility and sexual health. - Get treated immediately. If you test positive for a bacterial STI such as gonorrhea or chlamydia, the chances of long-term issues are decreased significantly if you can treat them right away. (It’s typically a simple course of antibiotics.)
- Freeze your sperm. We don’t know what might happen in the future. Freezing a healthy sperm sample ensures that no matter what happens, you’ll have choices for your future family.
- Test your fertility. If you have a history of sexually transmitted infection, sperm testing will help you understand any impact it may have on male fertility.
We highly recommend that, if you are considering sperm freezing or doing a semen analysis with the possibility of freezing sperm afterward, you complete STD testing first. Learn more.

Cost of STI testing
The cost of comprehensive STD screening can be up to $350, depending on your insurance plan and how many tests you complete. It typically also requires a doctor or clinic visit, which may come with its own fee.
Legacy’s mail-in STI testing kit offers you the option to test for 6 common STIs without leaving home, for $150. This test requires no doctor prescription or visit, and can be used even by those without insurance.
STI testing for males usually involves a blood test and a urine test, and could include a swab of the urethra or genitals. Legacy’s STI testing kit uses a blood and urine sample produced at home. Our STI testing kit provides peace of mind, helping you take your reproductive health in your own hands.
How can I check my own fertility?
If you’ve had a sexually transmitted infection in the past or you just want to understand your male fertility health now, sperm testing is the best place to start. Known as semen analysis, sperm testing typically measures sperm count (how many sperm you’re producing), plus sperm motility (how well sperm are moving) and morphology (how many sperm are the proper size and shape).
Legacy’s at-home semen analysis kits evaluate all of these key metrics, just like a fertility clinic — without the discomfort of visiting a sperm “collection room.” It’s easy: you produce your sample at home via masturbation and mail it to our CLIA-certified lab for analysis by a team of experienced scientists. In less than 48 hours, you’ll receive results that are reviewed by our medical staff.



