Trans and gender non-conforming (TGNC) people with sperm may be interested in having kids later in life, or simply don’t want to lose the option. Therefore, the question of fertility recovery after gender-affirming hormone therapy becomes paramount.
However, the chances of fertility recovery after stopping GAHT aren’t straightforward, and can be impacted by duration and dosage of hormones taken, the patient’s age when they started and stopped taking hormones, and their pre-existing fertility status.
Key takeaways
- Understanding the chances for fertility recovery after gender-affirming hormone therapy helps trans women and gender non-conforming people with sperm make informed decisions about their reproductive future and treatment options.
- Gender-affirming hormone therapy typically suppresses sperm production within 3–6 months.
- Fertility recovery is not guaranteed. Only 64% of trans women recover some fertility after stopping treatment, most have reduced fertility compared to before GAHT, and recovery timeframes vary dramatically from several months to over 2 years.
- Pausing hormone therapy causes reversal of feminizing effects and potential return of gender dysphoria, creating significant psychological distress.
- Sperm banking before starting hormone therapy offers the most reliable fertility preservation option, eliminating the need to interrupt GAHT later.
The impact of gender-affirming hormone therapy on sperm production
Gender-affirming hormone therapy (GAHT) changes reproductive functions in trans women through several biological pathways. Estrogen and anti-androgens lower testosterone levels and inhibit the hypothalamic-pituitary-gonadal axis, typically resulting in azoospermia (absence of sperm) within 3–6 months.
Mechanism of estrogen and anti-androgens in GAHT
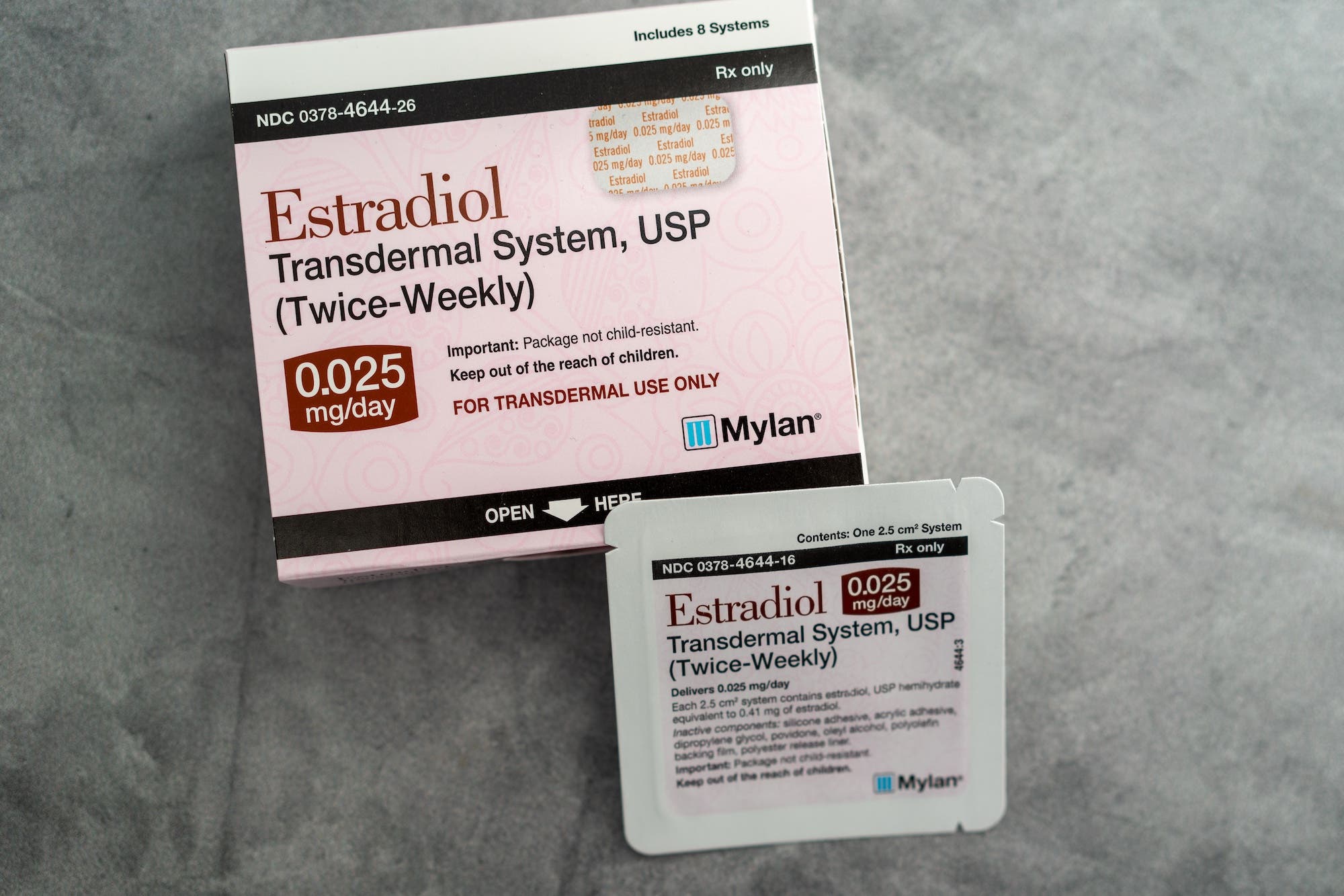
Feminizing hormone regimens typically combine estrogen with testosterone-blocking medications. Estrogens (like estradiol) bind directly to receptors throughout the body, suppressing the hypothalamic-pituitary-gonadal (HPG) axis through negative feedback mechanisms. Anti-androgens such as spironolactone, cyproterone acetate, or GnRH agonists either block testosterone receptors or stop testosterone production completely.
Suppression of spermatogenesis in trans women
These medications disrupt spermatogenesis (sperm production) in stages after treatment begins:
- First, a patient will experience decreased gonadotropin release (FSH and LH) from the pituitary gland. FSH and LH are responsible for sperm and testosterone production.
- Next, a patient will see a reduction in intratesticular testosterone levels.
- Sertoli cells are necessary for the process of sperm production, which takes place in a structure called the seminiferous tubules in the testes. The changes outlined above can cause a disruption in the function of Sertoli cells and the seminiferous tubules.
- Finally, altered hormone levels can cause impaired spermatogonial development and maturation.
Feminizing hormone regimens typically lead to oligospermia (low sperm count) or azoospermia (complete absence of sperm in ejaculate) within 6 months. Due to impaired sperm development, any remaining sperm often shows reduced motility (ability to swim) and abnormal morphology (size, shape, and structure of sperm), further reducing fertility potential.
Duration of hormone use and reproductive impact
Treatment duration directly relates to reproductive changes. The effects start within weeks, but complete spermatogenic suppression usually takes several months. Research shows that stopping GAHT within 6 months might allow quick fertility recovery. However, longer treatment creates bigger challenges.
Studies reveal lower rates of complete spermatogenesis recovery in people who use GAHT beyond 2–3 years. Some individuals experience permanent changes in testicular architecture. Still, reproductive outcomes vary greatly among individuals based on age, pre-treatment fertility status, medication types, and dosages used during transition.
Can trans women recover fertility after cessation of gender-affirming hormone therapy?
If a TGNC patient on feminizing hormones pauses their gender-affirming hormone therapy, can they recover fertility? Some impacts of GAHT, like voice changes and breast development, stay permanent. However, reproductive functions may come back partially for some people.¹
Spermatogenesis recovery after hormone cessation: what the research says
Research shows that about 64% of trans women recover some sperm production after they pause GAHT.² However, most GAHT patients are not able to recover their prior fertility parameters, and see lasting changes in their sperm characteristics, including reduced sperm concentration, motility, and morphology.³
Timeframe for potential fertility return
For those who are able to recover fertility, sperm production typically takes 3–6 months to return. However, recovery times can vary significantly.⁴ Some patients need up to 2 years or more before sperm production starts again, especially if they’ve been on hormones for several years or more.⁵
Setting realistic timelines becomes crucial when planning a family — and especially when working with GAHT patients. Taking a break from GAHT to recover fertility comes with real challenges, and patients might experience reversed feminizing effects and gender dysphoria. That’s why preserving fertility before treatment works better for many patients.
Legacy is a gender-inclusive sperm freezing option with a team that’s been trained in transgender care. Want to learn more about referring trans femme patients to Legacy?
Factors influencing fertility recovery after gender-affirming hormone therapy
Several things affect how well fertility might come back:
- Time spent on hormone therapy (longer use means lower chances of recovery)
- Patient’s age when stopping (younger people tend to recover better)
- Original fertility before starting GAHT
- Type of hormone treatment used (GnRH agonists vs. other anti-androgens)
Case studies of sperm recovery post-GAHT
In one study, a 26-year-old trans patient’s sperm production returned 6 months after stopping estradiol and spironolactone treatment that lasted 3 years.⁶
However, another patient showed no signs of spermatogenesis recovery after pausing the same treatment — estrogen and spironolactone — that they’d been taking for 5 years.⁷
Limitations in existing clinical data
The current research on fertility recovery after GAHT has its limits. We need more extensive, long-term studies because the existing ones have small sample sizes and irregular follow-ups. This would help trans women make better informed decisions about their reproductive options.
Studies are small, follow-up times vary, and hormone treatments differ between cases.⁸ Most research looks at short-term results instead of long-term reproductive abilities.
There may also be a use for medications traditionally used for male fertility, such as clomiphene citrate (Clomid) or hCG, to recover sperm production more quickly in trans women who desire parenthood. This area remains under-studied at the moment.
Complications of pausing gender-affirming hormone therapy
The idea of pausing gender-affirming hormone therapy to recover fertility is more complex than the simple medical research. As clinicians, we need to balance a patient’s reproductive goals with their desire to live as their authentic selves and avoid dysphoria. If a patient pauses gender-affirming care, they’ll experience a reversal of many of the feminizing effects of their therapy.
Reversal of feminizing effects of estrogen
Some feminizing effects of estrogen GAHT will gradually reverse after pausing therapy.⁹ Emotional changes can surface within 4–6 weeks as hormone levels change.¹⁰ The physical changes follow a common pattern:
- Within the first 1–3 months, the patient’s skin may become less soft. Body and facial hair might return to its original growth patterns.
- Over the next 3–6 months, body fat may move back to its original patterns. Breast size may decrease slowly, though some changes stay permanent.
It is common for patients to experience substantial distress from these physical and emotional changes.¹¹ Gender dysphoria often becomes more intense as feminine features reverse.¹²
Gender-affirming care patients who have to pause therapy commonly experience:
- Increased anxiety and depression
- More dissatisfaction with their body
- The desire to avoid social interaction as their appearance changes
- Disruption in how they express their gender identity
Affirming, inclusive mental health is crucial during this time. Clear information about expected changes and their timing helps patients cope better.
Fertility preservation prior to gender-affirming hormone therapy: A better way
Proactive fertility preservation represents the optimal approach, allowing trans women to maintain continuous gender-affirming care while preserving their reproductive options for the future.
Sperm banking before beginning GAHT offers the best approach to preserve fertility.⁸ This early planning lets patients store reproductive material so they can pursue parenthood without stopping hormone therapy later.⁷
The steps include:
- Providing samples through masturbation — with Legacy, this step can be done at home
- Testing sperm quality in an andrology lab to ensure the sample is a good candidate for freezing
- Cryopreserving sperm using liquid nitrogen to bring the cells to -196ºC
- Storing the sperm long-term for future use in fertility treatment like intrauterine insemination (IUI) or in vitro fertilization (IVF)
The benefits are clear, but many obstacles exist that can prevent trans women from freezing sperm. Typical costs run $1,000–$1,500 upfront, plus yearly storage fees. (Legacy is working to make this more affordable, with sperm freezing plans starting at $540.) Insurance doesn’t always cover fertility preservation for trans women.
Some areas lack easy access to affirming fertility care, and about 40% of the US actually lacks easy access to a fertility clinic at all.¹³ Legacy’s mail-in sample collection kit can help eliminate this barrier.
Frozen sperm can be stored for as long as desired without impacting its ability to create a healthy pregnancy. Preserved fertility material opens up several paths to parenthood:
- IVF or IUI with stored sperm and a partner’s eggs/uterus
- Gestational surrogacy arrangements
- Donor egg options combined with preserved sperm⁴
Studies have found that frozen sperm has roughly equivalent success rates to “fresh” never-frozen sperm when used in IUI or IVF techniques. Therefore, this approach works better than trying to restore fertility after treatment and helps avoid many complications.
For any TGNC patient with sperm, the first, most vital step is talking with doctors who understand both gender-affirming care and fertility. This helps create customized solutions for each person’s journey. Legacy is here to be your fertility resource.
Legacy is a gender-inclusive sperm freezing option with a team that’s been trained in transgender care. Want to learn more about referring trans femme patients to Legacy?
References
- 1. James et al. “The Report of the 2015 U.S. Transgender Survey,” 2016.
- 2. Coleman et al. “Standards of Care for the Health of Transgender and Gender Diverse People, Version 8,” 2022.
- 3. Ethics Committee of the American Society for Reproductive Medicine. “Access to fertility services by transgender and nonbinary persons: an Ethics Committee opinion,” 2021.
- 4. Auer et al. “Desire to Have Children Among Transgender People in Germany: A Cross-Sectional Multi-Center Study,” 2018.
- 5. Pew Research Center. “2023 PEW RESEARCH CENTER’S AMERICAN TRENDS PANEL,” 2023.
- 6. Rafferty et al. “Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents,” 2018.
- 7. American Psychological Association. “Guidelines for Psychological Practice With Transgender and Gender Nonconforming People,” 2015.
- 8. Walker et al. “Thoughts and opinions about fertility preservation and family building from the transgender community—an interview-based approach,” 2024.