April 18–24, 2021 is National Infertility Awareness Week, a time for education, advocacy, and support-building around the infertility community. Infertility affects 1 in 8 heterosexual couples. It’s a disease that’s diagnosed when a couple has been actively trying to conceive for 6–12 months or more, or has other issues affecting their ability to get pregnant naturally.
These are the top five male fertility myths, debunked—and everything you need to know about infertility.
Male fertility myth #1:
“Infertility is a female issue.”
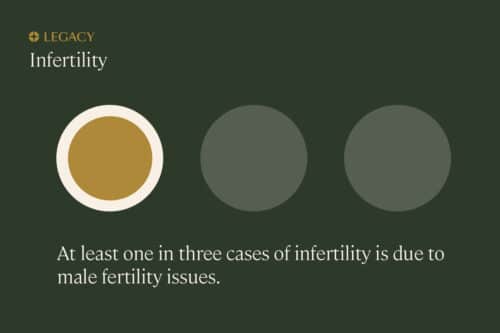
For too long, women have shouldered all the responsibility for fertility planning—and all of the blame, when trying to conceive didn’t go as planned. But the reality is that male-factor infertility accounts for around 1/3 of infertility cases; female-factor infertility accounts for another 1/3, and a combination of factors or “unknown” comprises the rest.
That means that around half of all infertility cases involve the male partner in some way. And this number is on the rise, as sperm counts drop globally. Between 1973 and 2011, sperm concentration declined 50–60% among Western men. Plus, paternal age is on the rise, and sperm quality decreases with age, especially after 40 (more about that below).
Fertility is far from a “women’s issue,” and framing it that way not only places undue pressure on the female partner, but creates shame and isolation amongst men who deal with infertility. Learn more in our Guide to Male Fertility.
Male fertility myth #2:
“Men are fertile at any age.”
Stories of men in their 60s or even older fathering children tend to fuel the idea that male fertility is eternal. After all, the world’s oldest dad was able to father a baby at 96 years old—so male fertility is eternal, right?
But that’s a misconception. While men typically continue producing sperm until death, paternal age is among the most significant factors affecting a couple’s chance of conceiving and their pregnancy outcomes. Men over the age of 35–40 typically experience a decrease in sperm health, affecting pregnancy rates, time to conception, miscarriage risk, adverse pregnant outcomes, and offspring health risks.
| Metric |
Effect of age |
| Pregnancy rates |
Men will generally see a 52% decrease in fertility rate between their early 30s and their mid-to-late 30s. |
| Time to conception |
Compared to men 25 years or younger, men 45 years or older are 12.5 times more likely to take over two years to conceive. |
| Miscarriage risk |
Pregnancy loss between the 6- and 20-week gestation period increases by 27% in fathers 35 years or older. That risk doubles when fathers reach 50. |
| Adverse pregnancy outcomes |
Pregnancies that involve a male over the age of 45 see an increased risk of birthing complications, and their offspring have an increased risk for adverse birth outcomes. |
| Offspring health risks |
Older fathers may be more likely to have children with schizophrenia, bipolar disorder, autism, Down syndrome, or childhood leukemia. |

There are four sperm quality parameters that change naturally with age: count, motility, morphology, and DNA fragmentation:
-
- Sperm count (how many sperm you have): Decreases 2.6% per year
- Motility (how well your sperm move): Decreases 0.8% per year
- Morphology (how many sperm are properly shaped): Decreases by 0.65% per year
- DNA fragmentation (damage to the DNA inside sperm): Increases by 0.3% per year
Bottom line: Men may keep making sperm for their whole lives, but the quality of that sperm changes measurably as they get older, and especially after age 35. Learn more about age and male fertility.
Male fertility myth #3:
“A man’s lifestyle doesn’t affect his fertility.”
We know that the partner who’ll be carrying the baby will need to change their lifestyle—no drinking, no smoking, and even some lunch meats are off-limits for pregnant women. But what about the partner whose sperm contributes half the baby’s genetic material?
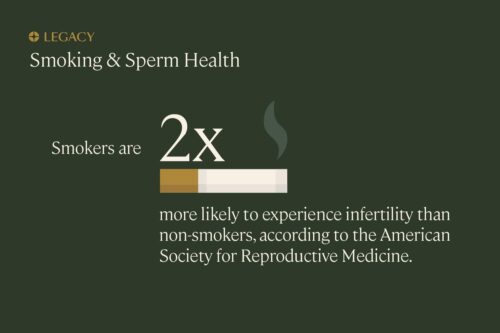
It turns out that a man’s lifestyle may have a significant impact on his semen parameters and sperm health. Especially smoking cigarettes. The American Society for Reproductive Medicine estimates that smokers have twice the risk of infertility, compared to non-smokers the same age. We also know, according to robust research, smoking is associated with significantly reduced sperm count, motility, and morphology.
And smoking isn’t the only lifestyle factor that can affect your fertility. Pretty much everything you do or consume—from your diet, to your alcohol intake, to how many hours of sleep you get each night—may impact your sperm quantity and/or quality. Since sperm takes about 72 days to produce, it’s important that you start to think about transitioning to a healthier lifestyle (if you’re not already there!) approximately 2–3 months before trying to conceive, so you can help create the healthiest possible pregnancy.
Learn more about improving your sperm.
Male fertility myth #4:
“Low sperm count or semen parameters means I’ll never be able to get my partner pregnant.”
Getting a semen analysis is a great first step to understanding your sperm health and your fertility. A semen analysis will reveal your semen parameters—semen volume, sperm count, concentration, motility, and morphology—and where you fall on a range from below average to above average.
But no semen analysis, even one as precise as Legacy’s, can tell you if you’re infertile (or not). That’s because infertility is what doctors call a “functional diagnosis.” You’re not considered infertile unless you’ve actually tried, and been unable to, conceive a child. While your semen parameters correlate with fertility outcomes—such as pregnancy rates, time to conception, and miscarriage rates—they’re just one piece of the reproduction puzzle.
Case in point: Even men with as low as 0% normal morphology have been able to produce a natural pregnancy. And while those with low sperm count have a lower chance of conception, they still have a 71% chance of getting their partner pregnant within 6 months of trying, according to one study.
Plus, semen parameters are not static. In most cases, poor semen parameters can be improved with some fairly simple lifestyle interventions: quitting smoking, improving your diet and exercise, or trying supplements for male fertility may all have a positive effect on fertility. Legacy clients get personalized lifestyle recommendations for improving their sperm health alongside their semen analysis report.
Male fertility myth #5:
“The only solution to male infertility is getting a sperm donor.”
Not quite. In 2021, there are many, many treatment options for male-factor infertility. First, we have the aforementioned lifestyle interventions. Experts estimate that most cases of male infertility can be addressed easily and cheaply, through lifestyle improvements or behavioral changes.
If the problem persists, there are a few fertility treatments that can help compensate for low sperm count or poor sperm quality. Intrauterine insemination or IUI is one example. During IUI, sperm is “washed” to isolate it from semen, and inserted directly into the uterus to give it a higher chance of resulting in fertilization. For severe cases of male-factor infertility, in vitro fertilization (IVF) with intracytoplasmic sperm injection (ICSI) may help. IVF is the process of fertilizing an egg in the lab; when using ICSI, a single sperm is injected directly into the egg to aid in fertilization.
There are other options for improving the chances of conception, based on what the cause of the infertility may be. For example, if a man has poor sperm quality or high sperm DNA fragmentation due to a varicocele (swollen veins in the scrotum), surgery reliably reverses the impact. If a man has azoospermia due to a blockage in his vas deferens, the tube that brings sperm from the testicles to the urethra—or because he was born with a vas deferens—doctors can retrieve sperm directly from his testicles, in a procedure known as a testicular sperm extraction or aspiration. Then, they’ll use that sperm in IVF with ICSI.
Today, there are many, many options for men dealing with infertility. To get a headstart on understanding your fertility, try an at-home semen analysis.